Consortium Psychiatricum
2023. Vol. 4, no. 2, 21–39
doi:10.17816/CP6132
ISSN: 2712-7672 / 2713-2919 (online)
Risk Factors of Disordered Eating in Adolescent Girls from a Community Sample: a Multidimensional Approach
Abstract
BACKGROUND: Eating disorders (ED) are severe, chronic, and complex in nature mental illnesses that are difficult to treat. One of the ways to stave off EDs is by screening among adolescents to preempt the development of clinical forms of ED in risk groups.
AIM: 1) to investigate the prevalence of ED risk among adolescent girls and compare subgroups at high and low risk of ED; 2) to investigate using a multidimensional approach those variables that can interact with temperament and character traits to predict ED symptomatology.
METHODS: The cross-sectional observational self-report study of a community sample of adolescent girls 12–17 years old (n=298; M=14.77±1.13) was carried out in the city of Ryazan, Russia. The Russian versions of Eating Attitudes Test and Cloninger’s Temperament and Character Inventory-Revised were used. In addition, an original questionnaire (Risk Factors of Eating Disorders) was developed. Regression models (to test for significant moderation) and path analysis (to test for significant mediations) were used.
RESULTS: Girls at risk of developing EDs are characterized by a heightened level of concern about weight and dissatisfaction with their body, tend to suffer from low self-directedness, higher novelty seeking and tendency to higher harm avoidance, display high alexithymia, experience self-distrust, negative emotionality and are dissatisfied with family relationships. They also suffer from low self-esteem and tend to be perfectionism and engage in risk behavior. Significant moderating effects were uncovered between the following ED risk factors: (1) self-distrust/risk behavior and BMI; (2) alexithymia/negative emotionality/self-esteem and cooperativeness; and (3) negative emotionality/risk behavior and self-transcendence. Family relationship dissatisfaction mediates the association between self-directedness/cooperativeness/self-transcendence and disordered eating.
CONCLUSION: There are various mutual influences between the numerous ED risk and prevention factors, which all together determine the paths between the predictors and final outcome.
General Information
Keywords: eating disorders, screening, adolescent girls, EAT-26, risk factors, personality, temperament and character
Journal rubric: Researches
Article type: scientific article
DOI: https://doi.org/10.17816/CP6132
Received: 27.03.2023
Accepted:
For citation: Meshkova T.A., Mitina O.V., Aleksandrova R.V. Risk Factors of Disordered Eating in Adolescent Girls from a Community Sample: a Multidimensional Approach. Consortium Psychiatricum, 2023. Vol. 4, no. 2, pp. 21–39. DOI: 10.17816/CP6132.
Full text
INTRODUCTION
Eating disorders (ED) such as anorexia nervosa (AN) and bulimia nervosa (BN) are severe mental illnesses that are difficult to treat [1, 2]. Their prevalence has not decreased, despite the large number of studies that have looked into the prevention and treatment of these diseases [3–5]. Both diseases are chronic and complex in nature [6, 7]. Some of the main risk factors for AN and BN are female gender and adolescence or early adulthood [4, 8–10]. The next on the list of leading risk factors is body image dissatisfaction [8, 11–14].
Clinical forms of ED have a pre-existing period, usually beginning in adolescence, that is characterized by a marked concern with body shape and weight and attempts to try various diets or purge, as well as an intense focus on physical fitness to avoid weight gains [7, 8, 12, 15]. What’s more, the risk of developing EDs increases as a result of social pressure from family, peers, and the media, which idealize the thinness of the female figure, instilling the idea that a beautiful figure of a woman is key to her success in life [16–18]. Recent cohort and longitudinal studies have shown that symptoms of ED that begin in adolescence, even if they do not morph into clinical ones, persist into early adulthood and lead to a greater risk of developing anxiety, depressive disorders, and obesity [19, 20].
One of the ways to prevent EDs is by conducting screening among adolescents girls especially in order to stave off the development of clinical forms of ED in risk groups [21, 22], even though, as recent studies have shown, conclusive evidence that such screening has benefits or does harm does not yet exist [4, 23]. Nevertheless, the ability to detect early disordered eating behavior which has not yet assumed pathological forms is of value not only to medical staff, but also to psychologists and teachers at secondary educational institutions. It is known that preventive programs, among them media literacy and healthy weight programs, cognitive-behavioral therapy, and cognitive dissonance interventions, can significantly reduce ED risk factors [24–26]. What we know about the trajectory of ED symptomatology development from early adolescence to adulthood allows us to conclude that ED prevention should start before puberty [27].
Despite the socio-cultural pressure that all adolescent girls, to some extent, experience, the risk of ED does not affect many of them. This has to do with the multifactorial nature of ED. Behavioral genetics research shows that there is a hereditary predisposition to develop these disorders [6, 28, 29]. Moreover, the particular environmental context can also reduce or increase the risk of ED [30]. Among those environmental factors, one of the most significant is family dynamics [31–34]. Some characteristics of one’s personality may or may not predispose them to ED [35–38].
It should also be noted that biological, developmental, psychological, and socio-cultural risks and protective mechanisms form complex constellations that accompany the process of individual development [35, 39–41]. The more information we can collect on the interplay amongst many of the factors involved in an individual’s development of a particular eating behavior, the better we will be at understanding the mechanisms of ED genesis [42, 43]. It is especially important to understand how the risk of ED emerges in its preclinical stages, namely during adolescence; which groups of adolescents become vulnerable to ED, and if it is possible to identify those areas of mental development and environmental context through whose leverage we can affect the risk of ED [39, 40].
Among the psychobiological factors associated with ED are the individual traits of temperament and character [44–47]. Temperament is considered one of the predictors for developing psychopathology due to its biological background, including rather high heritability, early manifestation, and relative stability during development [48, 49]. For example, temperamental characteristics in early childhood may predict body dissatisfaction and ED symptoms in adolescence [50, 51]. Temperament is one of the early indicators that can point to the subsequent development of personality traits influenced by experience and context [49].
One of the best known is Cloninger’s multidimensional psychobiological model of temperament and character, which clinical observations have led him to develop. This served as the basis for the development of the Temperament and Character Inventory (TCI) [52], which has become the go-to tool in various studies related to the substantiation of the neurobiological foundations of personality development, including neurobiological and genetic studies of psychopathology [53–55].
The adequate diagnostic and differentiating properties of TCI make it a tool that is used in the study of mental and personality disorders, as well as in person-centered therapy [56–58]. The TCI used in ED studies indicates significant differences between ED patients and healthy controls [44, 59, 60]. Using the Cloninger’s seven temperament and character dimensions as indicators and applying latent profile analysis, significant differences among profiles and ED diagnoses were observed [45]. There are also indications that subclinical forms of disordered eating behavior also show an association with TCI indicators [37, 61, 62].
Not only temperament and character traits, but also a number of other personality traits show significant associations with disordered eating behavior. These include perfectionism [63, 64], alexithymia [65, 66], low self-esteem [67, 68], personal ineffectiveness [69, 70], negative emotionality [71, 72], and other features.
The multidimensional nature of ED, with many risk and protective mechanisms, encourages researchers to probe for any possible forms of interaction between these factors. By using various methods of multivariate analysis, we are able to assess the moderation and mediation effects of such interactions that offer different etiological and maintenance models of ED [41, 43, 73–76].
Aim of the current study
The main purpose of this research was to probe for direct and indirect relationships between Cloninger’s temperament and character traits and the risk of developing ED in a community sample of adolescent girls. We have used a multidimensional approach to investigate variables that can interact with temperament and character traits to predict ED symptomatology. In addition, we endeavored to compare subgroups at high and low risk of ED in terms of BMI, body dissatisfaction and weight preoccupation, as well as a range of personality traits and satisfaction with family relationships. We hypothesize that a multidimensional approach has the potential to spawn valid models with significant predictor potential of ED risk in adolescent girls.
METHODS
Study design
The cross-sectional observational self-report study of a nonclinical sample of adolescent girls (298 participants) was carried out in the city of Ryazan (Central region of the Russian Federation) from November 2009 to November 2010.
Sampling
Convenience sampling was adopted for the aims of this research.
Participants
Inclusion criteria: (1) adolescent girls aged 12 to 17 years, (2) attending Middle and High School, (3) consent of participants and their parents, and (4) absence of indications of diagnosed mental disorders (according to information received from the school administration).
Exclusion criteria: (1) refusal of the girl or her parents to participate in the study at any stage, (2) inappropriate responses to the validation items of the Temperament and Character Inventory, and (3) Body Mass Index (BMI) of more than 34 or less than 13.
Procedure
Prior to the start of the study, informed consent was obtained from the girls’ parents for participation of their daughters in the study. Beforehand, the girls received information about the aims and conduct of the study. They were also informed that they could withdraw from the study at any time.
The girls were asked to fill out three paper-and-pencil questionnaires with Likert scales: (1) The Eating Attitudes Test (EAT-26), with 26 items; (2) The Risk Factors of Eating Disorders (RFED) questionnaire with 55 items (Table S1 in the Supplementary); and 3) The Cloninger Temperament and Character Inventory (TCI-R, short form), with 140 items. The questionnaires were used to gauge eating attitudes and behavior, weight and body concerns, temperament and character, some personality traits, and dynamics in the family. The girls were also asked to indicate their height and weight and make some marks in a form with eleven 100-mm vertical lines (Dembo-Rubinstein Self-esteem Scale) to rate their health, happiness, appearance, and some other features (Figure S1 in the Supplementary).
The questionnaires were filled by the group of girls in a classroom environment during two lessons of 45 minutes with a break of 10–15 minutes.
Measures
1. Eating Attitude Test (EAT-26)
The Russian version of the Eating Attitudes Test (EAT-26) [77, 78] was used to assess the risk of ED. EAT-26 is a widely used self-report questionnaire for screening for symptoms of AN and BN in adults and adolescents [79]. The questionnaire includes 26 items, for all of which the respondent can choose one of six possible answers, from “never” to “always”. The answers “always”, “usually”, and “often” are scored as 3, 2, 1, respectively. The rest of the answers — “sometimes”, “rarely”, and “never” — are assigned a value of 0 points. Scoring for question 26 is reversed. The total scores on the questionnaire can vary from a minimum value of 0 points to a maximum of 78 points. Total score cutoff at or above 20 is usually used for identifying respondents with possible ED risk.
According to the factor structure proposed by the authors, EAT-26 has three subscales: (1) Dieting; (2) Bulimia and Food Preoccupation; and (3) Oral Control. However, there has been a number of studies indicating that for non-clinical populations of adolescents or students at colleges and universities, the three-factor model is not applicable [80, 81]. In the present study, we have some of the scores of the above-mentioned subscales, but also, based on the data of exploratory factor analysis (EFA), we have obtained new estimates in accordance with the 5-factor model, which more adequately describes our sample (see more details in the Statistical analysis section and in the Supplementary Table S2).
To analyze the effects of moderation and mediation, we used the EAT-26 total scores derived from the 6-point scoring system, which scored the answer “always” as 5 and answer “never” as 0 points, since EAT-26 variables have multiple outliers in the 4-point scoring system, reducing their fit to a normal distribution.
2. Cloninger Temperament and Character Inventory-Revised (TCI-R, short form)
To assess the traits of temperament and character, we used Cloninger Temperament and Character Inventory-Revised (TCI-R, short form) [52]. The original version of the questionnaire and permission to use it were obtained from the lead author. The translation was done with the help of an expert, a bilingual psychologist from the U.S. A reverse translation was also done by an independent translator. Currently, TCI is considered a tool for assessing the seven dimensions of personality in terms of the comprehensive biopsychosocial model applicable not only to the assessment of psychopathology, but also to the general population [55].
In accordance with Cloninger’s model, temperament involves four dimensions: Novelty Seeking (NS), Persistence (PS), Reward Dependence (RD), and Harm Avoidance (HA).
Individual differences of a higher level associated with the formation of personal characteristics relating to the relationship of a person to themselves, with society, and with the world as a whole constitute the three dimensions of character. Self-Directedness (SD) is a personality trait associated with the ability of an individual to be self-sufficient, responsible, and able to calibrate their behavior to their own goals and values; Cooperativeness (C) is associated with individual differences that explain human behavior in their interaction with others; for example, empathy, willingness to help, etc.; Self-transcendence (ST) describes individual differences in people's relationship with the world as a whole, their identification with something related to spirituality, and the desire to determine the meaning of a person’s existence in the world [55].
The original questionnaire contains 240 items, the first 140 of which can be used as a short form. The authors of the questionnaire allow the use of answers in the form of “agreement-disagreement”, as well as in the form of a Likert scale. We used a 3-point scoring system with the response options “true”, “somewhat true”, and “false”. A score of 1 was assigned to “false” responses and a score of 3 to “true” responses. Thus, the evaluation of each answer was done in points ranging from 1 to 3. The reverse items were evaluated in the opposite order.
3. Risk Factors of Eating Disorders (RFED) questionnaire
To assess the typical ED risk factors, we developed an original 55-item questionnaire (Risk Factors of Eating Disorders, RFED), which included eight scales aimed at assessing some personal characteristics, body dissatisfaction, and weight concerns, as well as questions to assess family relationships. The mentioned-above 3-point scoring system was used. Total scores were measured for each scale. A brief description of the mentioned scales is given below, and the entire questionnaire is presented in Table S1 (in the Supplementary).
Perfectionism, 7-point scale with Cronbach’s alpha 0.665 and statements such as “I love everything to be perfect”, “I would like to be honors-student”.
Alexithymia, 6-point scale with Cronbach’s alpha 0.802 and statements such as “Sometimes I can’t tell if I’m hungry or upset”, “Sometimes I get feelings I can’t define”.
Self-Distrust, 7-point scale with Cronbach’s alpha 0.771 and statements such as “I feel like I can’t achieve much in life”, “I don’t believe in myself”. This characteristic is comparable to the “ineffectiveness” of the Eating Disorder Inventory [82].
Negative Emotionality, 11-point scale with Cronbach’s alpha 0.847 and statements such as “I am often depressed”, “I always think long and hard about what is happening to me”, “I often cry”.
Risk Behavior, 4-point scale with Cronbach’s alpha 0.643 and statements such as “I would like to experience the thrill even at the risk of my life (for example, skydiving)”, “If I was offered a weak drug, I would risk trying”.
Body Dissatisfaction, 4-point scale with Cronbach’s alpha 0.804 and statements such as “I don’t like my body”, “I envy the looks of other girls”.
Weight Concerns, 8-point scale with Cronbach’s alpha 0.812 and statements such as “I think I can’t be happy until I lose weight”, “Weight affects my mood, self-esteem, well-being and self-confidence”.
Family Relationships Dissatisfaction, 8-point scale with Cronbach’s alpha 0.789 and statements such as “I think my family underestimates me”, “My successes at home are scarcely encouraged”, “In the family, I am often scolded for missteps and shortcomings”.
4. Dembo-Rubinstein method of self-esteem measurement
The Dembo-Rubinstein method of self-esteem measurement [83] was used. Respondents were asked to assess their own health, mind, creativity, memory, appearance, self-belief, will, determined character, authority among peers, level of physical fitness, happiness. As an analyzed variable the level of self-esteem was used as an average value from the measurements of all characteristics obtained. This assessment tool is presented in more detail in Figure S1 (in the Supplementary).
Statistical analysis
1. Descriptive statistics and assessment of scale reliability
Descriptive statistics was used to extract the general characteristics of the sample: age, body mass index, and other categorical and continuous variables. Observations with missing data were removed. Because a number of variables characterizing eating behavior had a significant skewness and kurtosis, it was decided to prioritize methods of nonparametric statistics.
Cronbach’s alpha was used for the assessment of the scale’s reliability for questionnaires with Likert scales (EAT-26, TCI-R, RFED).
2. Exploratory factor analysis (EFA)
As mentioned above, the three-factor model of EAT-26 is not applicable for adolescent nonclinical samples. In this regard, at the first stage, we decided to conduct an exploratory factor analysis to refine the model which could be adequate to our sample. We used the factor extraction method based on the method of principal component analysis of the correlation matrix with the Varimax rotation, with 3-, 4-, 5-, and 6-factor models tested according to an eigenvalue level higher than 1.0 and the scree plot. Factor loadings of less than 0.60 were discarded.
The method of principal component analysis of the correlation matrix with the Varimax rotation was also used to assess the reproducibility of the factor structure of TCI-R for the temperament and character scales separately, as well as for all seven scales. Factor models were tested in accordance with the expected number of questionnaire scales (Table S3 in the Supplementary).
3. Identification and comparison of contrast groups with high and zero risk of ED
In accordance with the generally accepted cut-off criterion for the EAT-26, groups of girls with high (EAT-26≥20) and zero (EAT-26=0) values of the total EAT-26 were identified. The 2x2 contingency table was analyzed with the Pearson’s chi-square test of independence of distribution of the proportions of girls with high and zero ED risk depending on the grade (7–8 and 9–11 grades).
4. Comparison of eating attitudes and behavior (EAT-26) in two age groups
To account for the differences between younger and older adolescents, the entire sample was divided into 2 age groups: 12–14 years old and 15–17 years old. Since the distributions of the EAT-26 scores do not meet the criteria of normality, age differences were assessed using the Mann-Whitney test.
5. Binary logistic regression analysis
The logistic regression analysis (Wald statistic) was performed to assess the effects of independent predictors — BMI, temperament, and character traits (TCI-R), personality traits, and dissatisfaction with family relationships (RFED) — on the binary dependent variable of high (EAT-26≥20) vs. zero (EAT-26=0) risk of ED. We used the Enter model of logistic regression analysis.
6. Correlation analysis
The Spearman correlation analysis was used to estimate how EAT-26 total, BMI, TCI-R, RFED and self-esteem characteristics relate to each other.
7. Moderation analysis
To identify any significant moderation of the influence of one variable on another, regression analysis with two independent variables was used, taking into account the multiplicative term between the independent variables. BMI and seven traits of temperament and character (TCI-R) were used as independent variables. The EAT-26 total score assessed on a 6-point scale was treated as a dependent variable and Self-Esteem and six personality measures (RFED — Perfectionism, Alexithymia, Self-Distrust, Negative Emotionality, Risk Behavior), as moderators.
8. Mediation analysis
Path analysis using EQS 6.4 soft was utilized to identify any significant mediation of the influence of one variable on another. BMI and seven traits of temperament and character (TCI-R) were used as independent variables. The EAT-26 total score assessed on a 6-point scale was treated as a dependent variable, and Family Relationships Dissatisfaction as a mediator variable.
We used the Statsoft Statistica v10.0 software for all types of analyses, except for EFA and the moderation analysis, which were analyzed using IBM SPSS Statistics, v.23. EQS 6.4 soft was used for mediation analysis.
RESULTS
Overall sample characteristics
The sample was made up of students from four general secondary schools of the city of Ryazan, Russia. Two hundred and ninety-eight girls from 12.3 to 17.3 years old, students in 7–11 grades, were selected based on the inclusion-exclusion criteria. The mean age of the participants was 14.77±1.13 years. Some 90.3% of the group had already experienced menstruations. The mean age of menarche was 12.7±0.9 years. Most of the sample consisted of girls in 7–8 grades (88 and 98, accordingly, for a total of 186). The smaller part of the sample was made up of students in grades 9, 10, and 11 (28, 41, and 43 persons accordingly, for a total of 112). BMI varied from 13.49 to 33.98. Mean BMI=19.49±3.16.
Eating attitudes and behavior characteristics
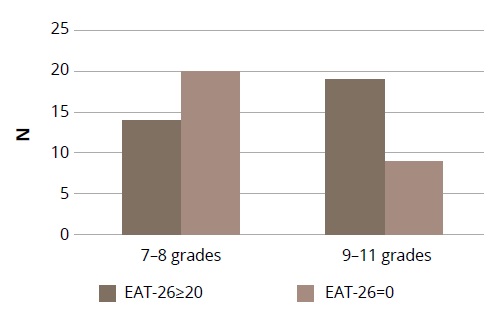
Thirty-three girls (11.1%) with total EAT-26 scores at or above 20 (risk group for ED) were identified. The contrast group with total scores of 0 consisted of 29 girls. A comparison of the proportion of girls with a risk and no risk of ED depending on their grade (7–8 and 9–11 grades) yielded significant differences by the 2x2 contingency tables: chi-square=4.39, df=1, p=0.036 (Figure 1).
Figure 1. The proportion of girls with high (EAT-26≥20) and low (EAT-26=0) ED risks depending on grade (7–8 and 9–11 grades).
Factor analysis results confirm the impossibility of reproducing the 3-factor structure proposed by the authors of the questionnaire. Seven eigenvalues >1 were obtained. In accordance with the Kaiser criterion, up to 7 independent factors can be considered. The most realistic for our sample seems to be a 5-factor model with the exclusion of items 2, 4, 5, 10, 15, 19, 22, 24, 26, which have low factor loadings (Table S2 in the Supplementary). The remaining items, all with factor loadings of more than 0.62, form 5 factors: (1) Drive for Thinness (items 1, 11, 12, 14, α=0.839); (2) Dieting (items 6, 7, 16, 17, α=0.868); (3) Social Pressure to Gain Weight (items 8, 13, 20, α=0.753); (4) Bulimia (items 9, 25, α=0.828); and (5) Food Preoccupation (items 3, 21, α=0.554).
To statistically evaluate the differences between younger and older adolescents, the entire sample was divided into two age groups: 12–14 years old and 15–17 years old. Since the distributions of the scales and the EAT-26 total score did not meet the criteria of normality, age differences were assessed using the Mann-Whitney test. A comparison of EAT-26 total and its three and five subscales demonstrated some significant differences between age groups (Table 1).
Table 1. Descriptive statistics of BMI and eating attitudes measured by the EAT-26 in two age groups of adolescent girls
|
Variables |
Age group (years) |
Mann-Whitney test |
||||||
|
12-14 (N=169) |
15-17 (N=129) |
12-14 (N=169) |
15-17 (N=129) |
12-14 (N=169) |
15-17 (N=129) |
|||
|
Min/Max |
Mean±SD |
Mean Rank |
U |
p |
||||
|
Age |
12.3/14.9 |
15.0/17.3 |
13.9±0.60 |
15.9±0.61 |
85 |
234 |
0.0 |
0.0001 |
|
BMI |
13.5/26.6 |
14.3/33.9 |
18.75±2.55 |
20.46±3.60 |
131.8 |
172.7 |
7912.0 |
0.0001 |
|
EAT-26 total |
0/42 |
0/47 |
7.01±7.47 |
9.26±10.09 |
142.7 |
158.39 |
9753.5 |
0.119 |
|
Three factors model (EAT-26) |
||||||||
|
Dieting |
0/25 |
0/33 |
4.03±5.24 |
5.88±7.12 |
140.7 |
161.05 |
9411.0 |
0.041 |
|
Bulimia and Food Preoccupation |
0/6 |
0/10 |
0.32±0.95 |
0.79±1.85 |
142.5 |
158.6 |
9724.5 |
0.016 |
|
Oral Control |
0/20 |
0/14 |
2.66±3.54 |
2.60±3.29 |
148.9 |
150.3 |
10793.0 |
0.881 |
|
Five factors model (EAT-26) |
||||||||
|
Drive for Thinness |
0/12 |
0/12 |
2.15±3.36 |
3.44±4.07 |
137.9 |
164.7 |
8942.5 |
0.004 |
|
Dieting |
0/12 |
0/12 |
0.72±1.93 |
0.92±2.18 |
146.0 |
154.1 |
10305.5 |
0.270 |
|
Social Pressure |
0/9 |
0/9 |
1.69±2.50 |
1.37±2.35 |
153.3 |
144.5 |
10257.0 |
0.328 |
|
Bulimia |
0/0 |
0/4 |
0 |
0.05±0.39 |
148.5 |
150.8 |
10731.5 |
0.106 |
|
Food Preoccupation |
0/3 |
0/6 |
0.12±0.56 |
0.28±0.93 |
145.5 |
154.8 |
10221.0 |
0.051 |
The incidence of EAT26 values at or above 20 is higher in the 15- to 17-year-old group — 15.5% vs. 7.7% in the 12- to 14-year-old age group. Although the differences are not statistically significant, there is a trend towards significance (chi-square=3.43; p=0.064).
TCI-R characteristics
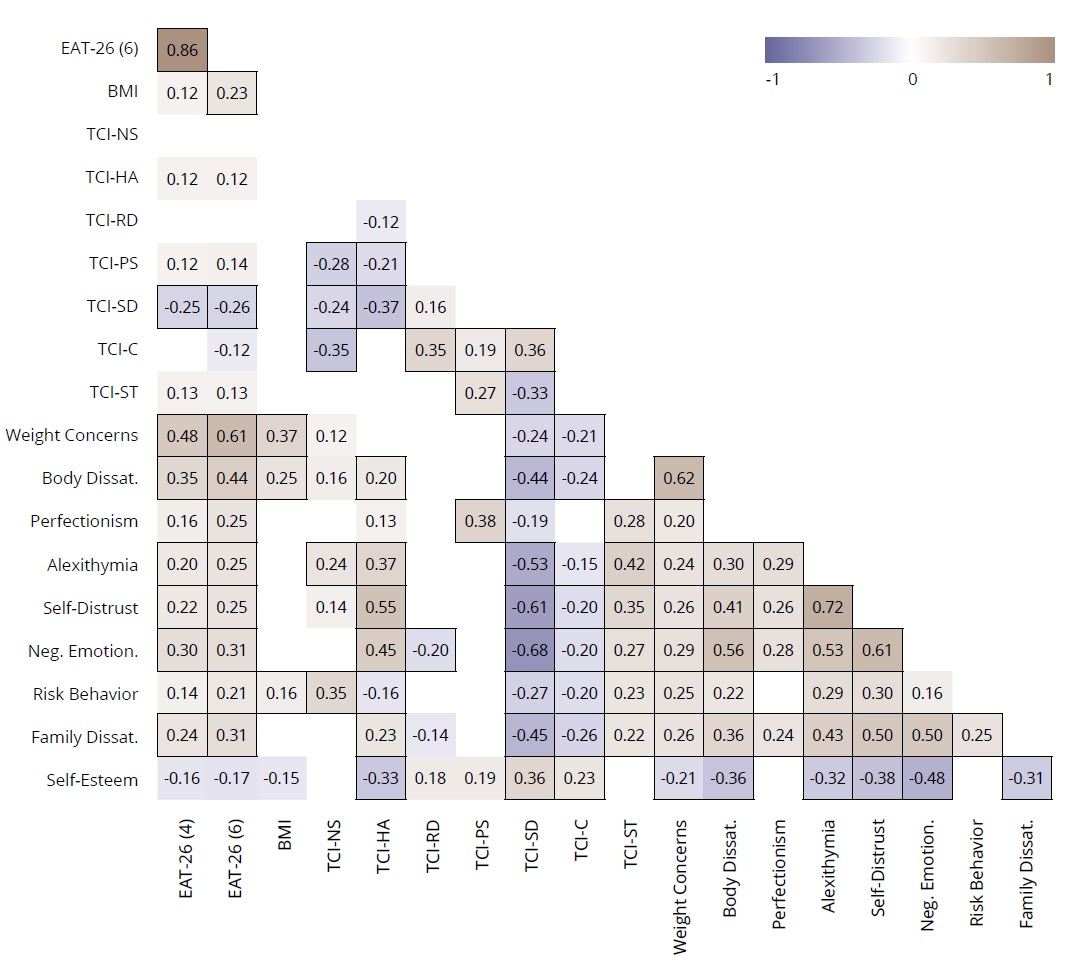
Basic statistics and the Cronbach’s alpha coefficients of seven TCI-R scales in the sample (N=298) are given in Table 2. The procedure used in exploratory factor analysis and factor loadings before and after rotation are presented in Table S3 (in the Supplementary). Cross-correlations between scales are presented in Figure 2.
Table 2. Temperament and Character scales characteristics
|
Scales |
Mean±SD |
Min |
Max |
Skewness |
Kurtosis |
Cronbach’s alpha |
|
Novelty Seeking |
40.53±5.75 |
26 |
56 |
0.127 |
-0.024 |
0.707 |
|
Harm Avoidance |
40.80±6.31 |
25 |
55 |
0.004 |
-0.480 |
0.754 |
|
Reward Dependence |
44.40±4.98 |
27 |
57 |
-0.483 |
0.178 |
0.584 |
|
Persistence |
40.81±7.04 |
22 |
58 |
-0.033 |
0.031 |
0.861 |
|
Self-Directedness |
45.09±6.47 |
25 |
58 |
-0.284 |
-0.157 |
0.789 |
|
Cooperativeness |
45.98±5.33 |
24 |
59 |
-0.831 |
1.164 |
0.697 |
|
Self-Transcendence |
31.31±5.97 |
16 |
46 |
0.122 |
-0.414 |
0.802 |
Figure 2. Correlation heatmap between EAT-26 total, BMI, TCI-R, RFED personality and self-esteem characteristics in the total sample
Note: EAT-26 (4) and EAT-26 (6) – total scores of EAT-26 derived from 4-point and 6-point scoring accordingly; statistically significant coefficients at p <0.001 are highlighted by frames.
Binary logistic regression analysis
Variables considered as probable and independent predictors of ED risk — BMI, temperament and character traits (TCI-R), personality traits, family relationship dissatisfaction (RFED), self-esteem — were included into the logistic regression analysis. The binary dependent variable was high (EAT-26≥20) or zero (EAT-26=0) risk of ED. The Wald statistics was used (Table 3).
Table 3. Independent predictors of high risk of developing eating disorders
|
Independent variables (predictors) |
Contrast groups N |
Wald statistic |
p |
|
|
EAT=0 |
EAT≥20 |
|||
|
BMI |
29 |
33 |
4.52 |
0.034 |
|
TCI (Temperament and Character Inventory) |
||||
|
Novelty Seeking |
29 |
33 |
5.13 |
0.023 |
|
Harm Avoidance |
29 |
33 |
3.23 |
0.072 |
|
Reward Dependence |
29 |
33 |
0.46 |
0.500 |
|
Persistence |
29 |
33 |
0.21 |
0.643 |
|
Self-Directedness |
29 |
33 |
10.65 |
0.001 |
|
Cooperativeness |
29 |
33 |
1.27 |
0.260 |
|
Self-Transcendence |
29 |
33 |
0.928 |
0.335 |
|
RFED (Risk Factors of Eating Disorders) |
||||
|
Weight Concerns |
28 |
33 |
19.76 |
0.0001 |
|
Body Dissatisfaction |
28 |
33 |
15.05 |
0.0001 |
|
Perfectionism |
28 |
33 |
3.06 |
0.080 |
|
Alexithymia |
28 |
33 |
5.30 |
0.021 |
|
Self-Distrust |
28 |
33 |
10.29 |
0.001 |
|
Negative Emotionality |
28 |
33 |
8.20 |
0.004 |
|
Risk Behavior |
28 |
33 |
3.66 |
0.056 |
|
Family Relationships Dissatisfaction |
28 |
33 |
5.66 |
0.017 |
|
Self-Esteem |
26 |
31 |
5.74 |
0.017 |
Based on the decrease Wald statistics principle, independent predictors of ED can be presented in decreasing order of predictive value as: (1) Weight Concerns, (2) Body Dissatisfaction, (3) Self-Directedness, (4) Self-Distrust, (5) Negative Emotionality, (6) Low Self-Esteem, (7) Family Relationships Dissatisfaction, (8) Alexithymia, (9) Novelty Seeking, and (10) BMI. Some variables with p-level <0.1 (Harm Avoidance, Perfectionism, Risk behavior) demonstrate a tendency toward significance.
Correlation analysis
Spearman correlations between EAT-26 total, BMI, TCI-R, RFED personality, and self-esteem characteristics were established (Figure 2). EAT-26 total was assessed on a 4-point scale and with the same assessment, but on a 6-point scale. The last estimation option was chosen as preferable due to the smaller number of outliers in the EAT-26 total distribution and was subsequently used to test the moderation and mediation models. It can be seen that many probable risk factors are also correlated with each other, which confirms that it is possible to detect the effects of moderation and mediation.
Moderation analysis
Over all, eight variables — BMI and seven TCI measures — have been considered as predictors; the EAT-26 total score assessed at a 6-point scale, as a dependent variable; and six personality measures (Perfectionism, Alexithymia, Self-Distrust, Negative Emotionality, Risk Behavior and Self-Esteem), as moderators.
To test for moderator effects, with EAT-26 total as the dependent variable, a subsequent series of linear multiple regressions were computed. Each independent variable, each moderator variable, and the product of the independent and moderator variable were entered into these regression analyses. The nature of each statistically significant interaction was examined with high and low representing the effects at 1 SD above the mean and 1 SD below the mean, respectively.
A total of 48 moderation models were analyzed, of which seven cases showed significant moderation effects (Table 4, Table 5).
Table 4. Summary of the regression analysis of all significant moderator effects
|
Parameters |
B |
SE B |
t |
p |
R2 |
|
Model 1. “BMI* Self-Distrust” |
|||||
|
Intercept |
31.953 |
19.109 |
1.672 |
0.096 |
0.180 |
|
BMI |
-1.258 |
0.980 |
-1.284 |
0.200 |
|
|
Self-Distrust |
-2.493 |
1.618 |
-1.541 |
0.124 |
|
|
BMI* Self-Distrust |
0.217 |
0.083 |
2.616 |
0.009 |
|
|
Model 2. “BMI* Risk Behavior” |
|||||
|
Intercept |
-34.655 |
18.984 |
-1.825 |
0.069 |
0.102 |
|
BMI |
2.596 |
0.959 |
2.706 |
0.007 |
|
|
Risk Behavior |
5.888 |
2.711 |
2.172 |
0.031 |
|
|
BMI* Risk Behavior |
-0.218 |
0.135 |
-1.610 |
0.108 |
|
|
Model 3. “Cooperativeness* Alexithymia” |
|||||
|
Intercept |
-27.780 |
31.495 |
-0.882 |
0.378 |
0.093 |
|
Cooperativeness |
0.851 |
0.669 |
1.272 |
0.204 |
|
|
Alexithymia |
6.141 |
2.539 |
2.419 |
0.016 |
|
|
Cooperativeness* Alexithymia |
-0.106 |
0.054 |
-1.943 |
0.053 |
|
|
Model 4. “Cooperativeness* Negative Emotionality” |
|||||
|
Intercept |
-43.042 |
36.823 |
-1.169 |
0.243 |
0.092 |
|
Cooperativeness |
1.141 |
0.787 |
1.450 |
0.148 |
|
|
Negative Emotionality |
3.728 |
1.511 |
2.467 |
0.014 |
|
|
Cooperativeness* Negative Emotionality |
-0.065 |
0.033 |
-1.997 |
0.047 |
|
|
Model 5. “Cooperativeness* Self-Esteem” |
|||||
|
Intercept |
177.208 |
52.187 |
3.396 |
0.001 |
0.075 |
|
Cooperativeness |
-2.874 |
1.135 |
-2.532 |
0.012 |
|
|
Self-Esteem |
-1.802 |
0.717 |
-2.511 |
0.013 |
|
|
Cooperativeness* Self-Esteem |
0.034 |
0.015 |
2.172 |
0.031 |
|
|
Model 6. “Self-Transcendence* Negative Emotionality” |
|||||
|
Intercept |
54.015 |
22.704 |
2.379 |
0.018 |
0.083 |
|
Self-Transcendence |
-1.455 |
0.739 |
-1.970 |
0.050 |
|
|
Negative Emotionality |
-1.337 |
0.947 |
-1.412 |
0.159 |
|
|
Self-Transcendence* Negative Emotionality |
0.067 |
0.030 |
2.241 |
0.026 |
|
|
Model 7. “Self-Transcendence* Risk Behavior” |
|||||
|
Intercept |
-23.853 |
16.830 |
-1.417 |
0.157 |
0.065 |
|
Self-Transcendence |
1.269 |
0.535 |
2.370 |
0.018 |
|
|
Risk Behavior |
6.476 |
2.485 |
2.606 |
0.010 |
|
|
Self-Transcendence* Risk Behavior |
-0.153 |
0.077 |
-1.981 |
0.048 |
|
Table 5. Intercept (A0) and linear regression coefficients (A1) at low and high values of moderators
|
Model |
Independent variables |
Moderators |
Levels of moderators and coefficients |
|||
|
Low |
High |
|||||
|
A0 |
A1 |
A0 |
A1 |
|||
|
1 |
BMI |
Self-Distrust |
12.12 |
0.47 |
-3.87 |
1.86 |
|
2 |
BMI |
Risk Behavior |
-6.43 |
1.55 |
16.56 |
0.70 |
|
3 |
Cooperativeness |
Alexithymia |
24.48 |
-0.05 |
64.50 |
-0.73 |
|
4 |
Cooperativeness |
Negative Emotionality |
23.89 |
-0.03 |
63.85 |
-0.72 |
|
5 |
Cooperativeness |
Self-Esteem |
68.24 |
-0.84 |
25.25 |
-0.04 |
|
6 |
Self-Transcendence |
Negative Emotionality |
30.00 |
-0.25 |
15.66 |
0.47 |
|
7 |
Self-Transcendence |
Risk Behavior |
7.19 |
0.54 |
32.48 |
-0.06 |
There are two significant interactions between BMI as predictor of disordered eating with such RFED parameters as Self-Distrust and Risk Behavior.
Three moderation effects were also uncovered as relates to the TCI character score Cooperativeness as an independent variable and Alexithymia, Negative Emotionality, and Self-Esteem as moderators.
The next independent variable for which significant moderation effects were identified was the TCI character score Self-Transcendence. For this independent variable, two significant moderators were found: Risk Behavior and Negative Emotionality.
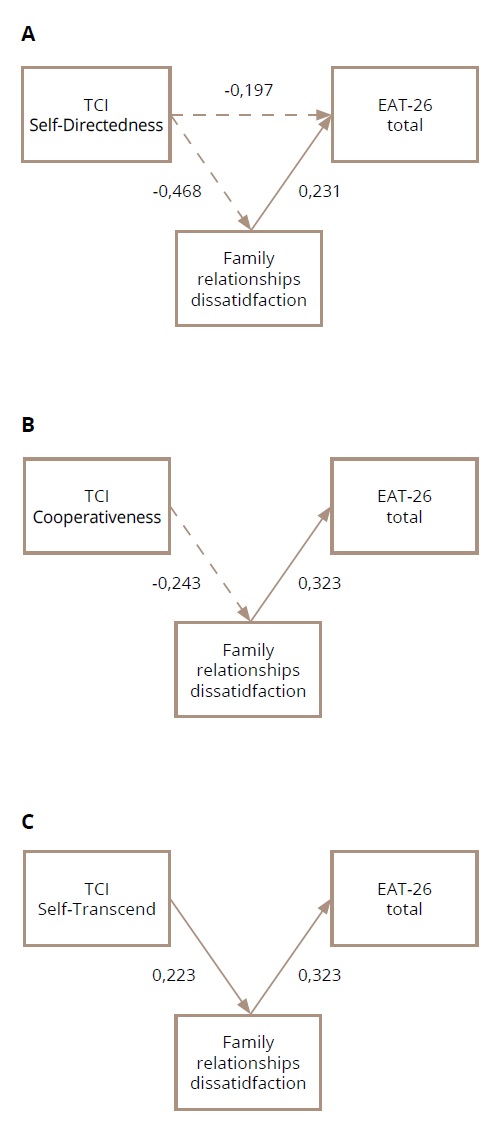
Mediation analysis
BMI and seven traits of temperament and character (TCI-R) were used as independent variables. The EAT-26 total score assessed on a 6-point scale was treated as the dependent variable, and Family Relationships Dissatisfaction as the mediator variable. All 8 mediation models were analyzed, of which three showed significant mediation effects. Three models with the TCI character traits SD, C, and ST as independent variables and Family relationship dissatisfaction as the mediator showed a good fit. The hypothesized relationships between three dimensions of character by the Cloninger’s TCI and Family Relationships Dissatisfaction as the mediator variable were statistically significant. The effects of C and ST on eating behavior (EAT-26 total scores on a 6-point assessment) are fully mediated by Family Relationship Dissatisfaction without the direct effects. SD demonstrates also a direct effect on the EAT-26 level: however, the effects through the mediation are more pronounced.
The results of the mediation analysis are presented in Figure 3 (A, B, C) and in Table S4 (in the Supplementary).
Figure 3. Graphic depiction of mediation models with Family Relationships Dissatisfaction as a mediator variable and Self-Directedness (A), Cooperativeness (B), and Self-Transcendence (C) as independent variables. Only significant effects are presented.
Note: A — All path coefficients are significant. The indirect effect is significant and equal to -0.078. This model is exactly estimated, so there are no fit indices; B — Fit indices: chi-square=2.582, df=1, p=0.108, CFI=0.969, RMSEA=0.073. 90% CI (0.0001; 0.188). All regression coefficients are significant. The indirect effect is significant and equal to -0.108; C — Fit indices: chi-square=1.369, df=1, p=0.242, CFI=0.992, RMSEA=0.035, 90% CI (0.0001; 0.163). All regression coefficients are significant. The indirect effect is significant and equal to 0.072.
DISCUSSION
Age differences in eating attitudes and behavior and prevalence of ED risk
The comparison of EAT-26 total and its three and five subscales showed some significant differences between age groups. There were no significant age differences in the total EAT-26 scores, but the Dieting scale of the traditional 3-factors model had higher scores in older girls (15–17 years old). But in the five-factor model, significant differences were observed only on the “Drive for Thinness” scale, while on the “Dieting” scale, which reflects the specifics of the eating behavior, the differences were not significant. This can be explained by the fact that the Dieting scale in the three-factor model includes items concerning both dieting and drive for thinness. It is likely that the age differences in the dieting scale scores (three-factor model) are mainly due to those items related to weight concerns and drive for thinness.
In terms of one of the research questions concerning the prevalence of ED risk in adolescent girls from the community sample, the present study demonstrates that 11.1% of girls in all samples had EAT-26 scores at or above 20, which is evidence of a risk of ED. At the same time, comparison between the age groups of 12–14 and 15–17 years olds showed that the risk of ED was noticeably higher in the older age group (15.5% vs 7.7% in the younger group). The differences are not statistically significant, but there is a trend (p=0.064). This is consistent with the results of other investigations dealing with EAT-26 screening in adolescent samples [84].
The prevalence of ED risk as measured by EAT-26 varies greatly with age, gender, and region in which the study is conducted. Most contemporary reviews and meta-analyses are based on samples of university and college students [85, 86]. In the only cross-cultural study [87] involving female students from Russia and Japan, 8.6% of the Russian respondents and 7.9% of the Japanese respondents appeared at risk. The differences are not statistically significant. The results for adolescents are lower. In many cases, the samples include not only girls, but boys as well. For example, it is reported that in a Greek sample of adolescent girls the occurrence of EAT scores that exceeded the cutoff level over the years were 24.7% (2011) [88], 19.3% (2017) [89], and 25–33% for boys and girls, depending on the BMI level (2021) [90]. For Hong Kong and Chinese adolescent girls, we can find estimates of ED risk at 6.5% (1996) [91], 26.6% (2011) [92], 27.1% (2017) [93], and 6.8% (2022) [94]. Among 15- to 19-year-old adolescent girls from the Kingdom of Saudi Arabia, disordered eating behaviors were established in 25.47% of participants in the study [95]. A systematic review and meta-analysis of child and adolescent mental health disorders in the GCC report on the pooled prevalence of disordered eating behavior tested by the EAT-26 as 31.55% [96]. The prevalence of disordered eating behavior in a Dutch cohort study on mental health and social development from preadolescence into young adulthood as reported by F.R. Smink et al. stood at 14–22% [97].
In the few community studies of adolescents’ eating attitudes and behavior conducted in Russia, an average of about 8–15% adolescent girls exceeded the cutoff [98, 99]. One study highlighted the significant influence of the school type factor. The ED risk was most pronounced in students at a prestigious linguistic gymnasium (21.4%) compared with students at ordinary schools (6%) [98]. On the whole, the prevalence of ED risk arrived at in this study is in line with the existing data on Russia and is generally consistent with the results of other studies involving high school adolescent girls in the West.
Assessment of putative predictors of ED risk
The logistic regression analysis of a sample of two subgroups with high (EAT-26≥20) and zero (EAT-26=0) risk of ED regarded as a binary-dependent variable made it possible to identify and rank some variables as putative predictors of ED risk. Among them the most potent effects were attributed to Weight Concerns and Body Dissatisfaction. The rank correlation coefficients between EAT-26 and the parameters of Weight Concerns and Body Dissatisfaction are also the biggest amongst other significant coefficients. These parameters may be considered as dominant risk factors. This fully consists with the previously reported data on the risk factors of ED [8, 11–13, 100, 101]. In a recent umbrella review of published meta-analyses, the risk factor of body dissatisfaction leading to ED was graded as suggestive [14].
At the same time, the effect of BMI on eating attitudes and behavior is much subtle and ranks last among all mentioned effects. The correlation coefficient between BMI and EAT-26 total is very low (0.18). This suggests that subjective perceptions of body image and weight in adolescent girls play a much more important role in the risk of developing ED as measured by EAT-26 than an objective indicator such as BMI. Generally, in studies of risk factors for ED among adolescents with reasonable weight, BMI shows a weak association and is not considered an important predictor of ED. However, in overweight and obese adolescents BMI becomes a more significant risk factor for ED [15, 90, 94, 102]. It should also be noted that the relationship between BMI and ED risk should be considered in the context of the risk of developing a specific disorder: AN, BN or binge eating disorder (BED).
With regard to temperament and character traits, statistically significant effects were identified for SD (p=0.001) and NS (p=0.023). There is also a trend towards significance in HA (p=0.072). Girls at high risk of ED have higher NS and HA and lower SD. SD seems to have the biggest effect. Correlations between SD and EAT-26 total are also the strongest, but they are negative. Many previous studies regarding the comparison of Cloninger’s temperament and character traits in individuals with ED and healthy controls have reported similar results [36, 37, 44, 60, 62, 103–105]. As a rule, low SD is not only characteristic of ED, but also of other psychopathologies [106, 107]. As for temperamental traits, the results of a meta-analysis show that higher NS values are typical of a BN diagnosis, only, while higher values of HA are characteristic of all types of EDs [46].
Among other personal characteristics that seem to have a significant impact, we can point to such traits as high Alexithymia (p=0.021), Self-Distrust (p=0.001), Negative Emotionality (p=0.004), and low Self-Esteem. (p=0.017). For the high Perfectionism and Risk Behavior categories, there are only tendencies towards significance (p=0.08 and p=0.056, accordingly). All of these features are among the known risk factors of ED, which has been confirmed by many studies [63–72].
Another variable that seems to have a significant weight is Family Relationships Dissatisfaction (p=0.017). Girls at risk are significantly more dissatisfied with the dynamics in their families. They believe that their parents underestimate them, treat them too harshly, often punish them for misconduct, do not notice their achievements, and so on. It is known that family factors are also considered important components in the system of risk and protection factors in the development of disordered eating behavior [31, 32, 34]. For example, adolescents diagnosed with Restrictive Eating Disorders are characterized by alexithymia, which comes with a pattern of dysfunction in family interactions, with a predominance of collusive alliances [33]. In a population-based longitudinal study of adolescents in Australia, an association was found between low levels of parental warmth and the risk of ED. The relationship was limited to girls, and low parental warmth was associated with bulimic behavior. As for the relationship between the dynamics in the family and body dissatisfaction and drive for thinness, there was a noticeable compounding effect between low parental warmth and low monitoring [108]. In a sample of Italian adolescent boys and girls, significant gender differences were also uncovered in the association between poor family dynamics and dysfunctional eating behavior: girls perceive their families as characterized primarily by a low level of flexibility [109].
Moderation and mediation models
The correlation between the EAT-26 total score and all prediction variables, in common with the correlation between all variables, demonstrates that many of the hypothesized risk factors also correlate with each other. This suggests that there may be more complex associations between variables that only a multivariate analysis can help reveal. Among all the moderation and mediation models we tested, several models demonstrated a good fit.
There are two significant interactions between BMI as a predictor of ED risk with Self-Distrust and Risk Behavior as a moderator. Adolescent girls who score high on Self-Distrust demonstrate a faster increase in EAT-26 total scores with an increase in BMI, than those whose Self-Distrust scores are on the low end. At the same time, the level of Risk Behavior has the opposite effect on the relationship between BMI and eating attitudes. Girls with a high level of Risk Behavior attitude show a weaker increase in EAT-26 total scores, with an increase in BMI. As mentioned above, BMI is a weak predictor of ED risk, in particular for people with normal weight, but we see that, when combined with a high degree of Self-Distrust or low level of Risk Behavior, the role of the BMI factor increases.
As already mentioned, C is also considered as weakly associated with ED, but its role increases in combination with factors such as a high level of Alexithymia or Negative Emotionality. At high levels of one or the other moderator, there is a noticeable negative relationship between C and EAT-26. The same effect was found for low Self-Esteem, another moderator. These results indicate the presence of complex relationships between psychobiological personality predictors and the risk of ED in the context of the moderation effects of other personality variables. The same goes for ST, which is also considered almost unrelated to the risk of ED. For this character trait, two moderation effects were also found for the variables Negative Emotionality and Risk Behavior. Girls with a high level of Negative Emotionality show a positive relationship between ST and EAT-26 total scores, whereas with a low level of Negative Emotionality we see an opposite consistent pattern. At a low level of Risk Behavior, there is an evident positive relationship between ST and EAT-26, while at a high level there is no relationship.
The C and ST items were also shown to be indirectly associated with ED risk through the mediation variable Family Relationships Dissatisfaction. This variable as a mediator also increases the positive association between low SD and ED risk.
The moderation and mediation models we have uncovered suggest that we are dealing with a complex system of interactions between many factors that can increase or decrease the risk of ED in adolescents. Evidence is accumulating pointing to the complex effects of risk-protection interactions in relation to the study of the genesis of adolescent ED. For example, high self-esteem appears to be a protective factor when the girls possess a high degree of perfectionism [110]; self-oriented perfectionism partially mediates the relationship between body dissatisfaction and disordered eating behavior [111]; body shame partially mediates the relationship between body dissatisfaction and eating behavior [112]; stress and attachment anxiety predict emotional eating through rumination [113]; gender significantly moderates the relationship between anxiety symptoms and EAT bulimia subscale scores, but BMI does not [114]; perceived peer support seems to have a moderation effect on the relationship between a father’s psychological control and negative eating attitudes and behaviors [115]; daytime sleepiness mediates the relationship between internalizing symptoms and disordered eating [116]; emotional eating and cognitive restraint mediates the relationship between difficulties in emotion regulation and perfectionism and ED symptoms [117]; and many more. Indeed, further research into the moderators or mediators involved in the system of risk or protective factors regarding adolescent ED risk is required.
Unfortunately, there are no similar studies on the effects of moderation and mediation of the relationship between temperament and character traits and adolescent eating behavior. However, there is some information regarding studies with adult participants. Serial mediation analyses showed that association between HA and body dissatisfaction in women with BN is fully mediated by two significant, indirect effects through low self-esteem and through depression and low self-esteem in serial [118]. It was also shown that the association of high HA and low SD with ED severity is mediated by difficulties in emotion regulation [119]. In one of the studies, it was found that temperamental traits seem to play a full mediating role in the relationship between puberty and ED severity: age of puberty increases the level of HA, which in turn increases the severity of ED [120].
In modern research, network-based methods for psychometric data are increasingly used, including in ED studies. In the network model, symptoms are conceptualized as interacting and mutually reinforcing elements in a complex network [2, 121, 122]. In one of these studies, performed in a sample of 2,302 treatment-seeking ED patients with different diagnoses, seven Cloninger’s TCI-R scales were also included among of the 32 features related to ED diagnoses [123]. The authors indicated that among all the symptoms of ED in question overvigilance, excessive focus on inhibiting emotions and feelings, interoceptive awareness, and perfectionism were critical. However, it should be pointed out that with this approach, when patients with fundamentally different diagnoses such as AN and BED are mixed, information is lost as regards the specifics of a particular disorder.
Strengths and limitations of the study
In the present study, for the first time in Russia, a multidimensional approach was applied to the study of the risk factors of eating disorders in adolescent girls, based on the psychobiological model of temperament and character of Robert Cloninger. In addition, an original questionnaire (Risk Factors of Eating Disorders) was developed. As a result, it was possible to identify several risk factors for ED associated with psychobiological, personal, and family factors, taking into account the effects of moderation and mediation.
One of the limitations of this study is its cross-sectional design, which does not allow for establishing a definitive relationship between the presence of one or the other risk factor and long-term consequences such as disordered eating. The second limitation is the absence of a standard validation procedure for some of the measuring instruments used in this study. In addition, it can be noted that all variables were obtained as a result of girls’ self-reporting, which could lead to inaccuracies in the estimates. Therefore, the results obtained can only be regarded as preliminary.
One of the possible directions to continuing this study may be the introduction of other anthropometric variables (not only BMI), which can be associated with an adolescent’s eating habits and reflect not only the actual values, but also the deviation of individual anthropometric measurements from their normalized values (percentiles, z-scores).
CONCLUSION
In general, it can be concluded that there are various interrelated influences amongst the numerous possible ED risk and prevention factors, which determines the paths between the predictor and the outcome. The better we understand these pathways, the more effectively it will be possible to plan the prevention and treatment of ED. It is of utmost importance to think about ways to stave off the risk of ED starting from childhood and adolescence.
Supplementary Material
References
- Steinhausen HC. Outcome of eating disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;18(1):225-42. doi: 10.1016/j.chc.2008.07.013.
- Monteleone AM, Pellegrino F, Croatto G, et al. Treatment of eating disorders: a systematic meta-review of meta-analyses and network meta-analyses. Neuroscience & Biobehavioral Reviews. 2022;142:104857. doi: 10.1016/j.neubiorev.2022.104857.
- Kaye WH, Bulik CM. Treatment of patients with anorexia nervosa in the USA crisis in care. JAMA Psychiatry. 2021;78(6):591–592. doi: 10.1001/jamapsychiatry.2020.4796.
- Attia E, Guarda AS. Prevention and early identification of eating disorders. JAMA. 2022;327(11):1029–1031. doi: 10.1001/jama.2022.2458.
- Bryant E, Spielman K, Le A. et al. Screening, assessment and diagnosis in the eating disorders: findings from a rapid review. Journal of Eating Disorders. 2022;10(1):78. doi: 10.1186/s40337-022-00597-8.
- Bulik CM, Blake L, Austin J. Genetics of eating disorders: what the clinician needs to know. Psychiatric Clinics of North America. 2019;42(1):59-73. doi: 10.1016/j.psc.2018.10.007.
- Filipponi C, Visentini C, Filippini T, et al. The follow-up of eating disorders from adolescence to early adulthood: a systematic review. International Journal of Environmental Research and Public Health. 2022;19(23):16237. doi: 10.3390/ijerph192316237.
- Jacobi C, Hayward C, de Zwaan M, et al. Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin. 2004;130(1):19-65. doi: 10.1037/0033-2909.130.1.19.
- Klump KL. Puberty as a critical risk period for eating disorders: a review of human and animal studies. Hormones and Behavior. 2013;64(2):399-410. doi: 10.1016/j.yhbeh.2013.02.019.
- Suarez-Albor CL, Galletta M, Gómez-Bustamante EM. Factors associated with eating disorders in adolescents: a systematic review. Acta Biomedica. 2022;93(3):e2022253. doi: 10.23750/abm.v93i3.13140.
- Littleton HL, Ollendick T. Negative body image and disordered eating behavior in children and adolescents: what places youth at risk and how can these problems be prevented? Clinical Child and Family Psychology Review. 2003;6(1):51-66. doi: 10.1023/a:1022266017046.
- Stice E, Marti CN, Durant S. Risk factors for onset of eating disorders: evidence of multiple risk pathways from an 8-year prospective study. Behaviour Research and Therapy. 2011;49(10):622-627. doi: 10.1016/j.brat.2011.06.009.
- McLean SA, Paxton SJ. Body Image in the Context of Eating Disorders. Psychiatric Clinics of North America. 2019;42(1):145-156. doi: 10.1016/j.psc.2018.10.006.
- Solmi M, Radua J, Stubbs B, et al. Risk factors for eating disorders: an umbrella review of published meta-analyses. Brazilian Journal of Psychiatry. 2021;43(3):314-323. doi: 10.1590/1516-4446-2020-1099.
- Rohde P, Stice E, Marti CN. Development and predictive effects of eating disorder risk factors during adolescence: Implications for prevention efforts. International Journal of Eating Disorders. 2015;48(2):187-98. doi: 10.1002/eat.22270.
- Bauer KW, Bucchianeri MM, Neumark-Sztainer D. Mother-reported parental weight talk and adolescent girls’ emotional health, weight control attempts, and disordered eating behaviors. Journal of Eating Disorders. 2013;1:45. doi: 10.1186/2050-2974-1-45.
- Jankauskiene R, Baceviciene M. Media pressures, internalization of appearance ideals and disordered eating among adolescent girls and boys: testing the moderating role of body appreciation. Nutrients. 2022;14(11):2227. doi: 10.3390/nu14112227.
- Zimmer-Gembeck MeJ, Hawes T, Scott RA, et al. Adolescents’ online appearance preoccupation: a 5-year longitudinal study of the influence of peers, parents, beliefs, and disordered eating. Computers in Human Behavior. 2023;140:107569. doi: 10.1016/j.chb.2022.107569.
- Herpertz-Dahlmann B, Dempfle A, Konrad K, et al. BELLA study group. Eating disorder symptoms do not just disappear: the implications of adolescent eating-disordered behaviour for body weight and mental health in young adulthood. European Child & Adolescent Psychiatry. 2015;24(6):675-84. doi: 10.1007/s00787-014-0610-3.
- Linardon J, Greenwood CJ, Fuller-Tyszkiewicz M, et al. Young adult mental health sequelae of eating and body image disturbances in adolescence. International Journal of Eating Disorders. 2021;54(9):1680-1688. doi: 10.1002/eat.23575.
- Kutz AM, Marsh AG, Gunderson CG et al. Eating disorder screening: a systematic review and meta-analysis of diagnostic test characteristics of the SCOFF. Journal of General Internal Medicine. 2020;35(3):885–893. doi: 10.1007/s11606-019-05478-6.
- Feltner C, Peat C, Reddy S, et al. Screening for eating disorders in adolescents and adults: evidence report and systematic review for the US preventive services task force. JAMA. 2022;327(11):1068–1082. doi: 10.1001/jama.2022.1807.
- US Preventive Services Task Force; Davidson KW, Barry MJ, Mangione CM, et al. Screening for eating disorders in adolescents and adults: US preventive services task force recommendation statement. JAMA. 2022;327(11):1061-1067. doi: 10.1001/jama.2022.1806.
- Stice E, Becker CB, Yokum S. Eating disorder prevention: current evidence-base and future directions. International Journal of Eating Disorders. 2013;46(5):478-85. doi: 10.1002/eat.22105.
- Le LK, Barendregt JJ, Hay P, Mihalopoulos C. Prevention of eating disorders: a systematic review and meta-analysis. Clinical Psychology Review. 2017;53:46-58. doi: 10.1016/j.cpr.2017.02.001.
- Shloido DE. Prevention of eating disorders: review of programs with proven effectiveness. Psychology. Psychophysiology. 2022;15(3):56–69. doi: 10.14529/jpps220306. Russian.
- Breton É, Dufour R, Côté SM, et al. Developmental trajectories of eating disorder symptoms: a longitudinal study from early adolescence to young adulthood. Journal of Eating Disorders. 2022;10(1):84. doi: 10.1186/s40337-022-00603-z.
- Meshkova TA. Heredity and Environment in Etiology of Eating Disorders. II. Review of Twin Studies. Clinical Psychology and Special Education. 2015;4(2):1–24. Russian.
- Himmerich H, Bentley J, Kan C, Treasure J. Genetic risk factors for eating disorders: an update and insights into pathophysiology. Therapeutic Advances in Psychopharmacology. 2019;9:2045125318814734. doi: 10.1177/2045125318814734.
- Klump KL, Wonderlich S, Lehoux P, et al. Does environment matter? A review of nonshared environment and eating disorders. International Journal of Eating Disorders. 2002;31(2):118-35. doi: 10.1002/eat.10024.
- Erriu M, Cimino S, Cerniglia L. The role of family relationships in eating disorders in adolescents: a narrative review. Behavioral Sciences. 2020;10(4):71. doi: 10.3390/bs10040071.
- Cerniglia L, Cimino S, Tafà M, et al. Family profiles in eating disorders: family functioning and psychopathology. Psychology Research and Behavior Management. 2017;10:305-312. doi: 10.2147/PRBM.S145463.
- Coci C, Provenzi L, De Giorgis V, et al. On behalf of the mondino foundation eating disorders clinical and research group. Family dysfunctional interactive patterns and alexithymia in adolescent patients with restrictive eating disorders. Children (Basel). 2022;9(7):1038. doi: 10.3390/children9071038.
- Langdon-Daly J, Serpell L. Protective factors against disordered eating in family systems: a systematic review of research. Journal of Eating Disorders. 2017;5:12. doi: 10.1186/s40337-017-0141-7.
- Leon GR, Fulkerson JA, Perry CL, et al. Three to four year prospective evaluation of personality and behavioral risk factors for later disordered eating in adolescent girls and boys. Journal of Youth and Adolescence. 1999;28:181–196. doi: 10.1023/A:1021649314458.
- Cassin SE, von Ranson KM. Personality and eating disorders: a decade in review. Clinical Psychology Review. 2005;25(7):895-916. doi: 10.1016/j.cpr.2005.04.012.
- Abbate-Daga G, Gramaglia C, Malfi G, et al. Eating problems and personality traits. An Italian pilot study among 992 high school students. European Eating Disorders Review. 2007;15(6):471-8. doi: 10.1002/erv.770.
- Dufresne L, Bussières EL, Bédard A, et al. Personality traits in adolescents with eating disorder: A meta-analytic review. International Journal of Eating Disorders. 2020;53(2):157-173. doi: 10.1002/eat.23183.
- Gicquel L. Anorexia nervosa during adolescence and young adulthood: towards a developmental and integrative approach sensitive to time course. Journal of Physiology — Paris. 2013;107(4):268-277. doi: 10.1016/j.jphysparis.2013.03.010.
- Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet. 2020;395(10227):899-911. doi: 10.1016/S0140-6736(20)30059-3.
- Zanella E, Lee E. Integrative review on psychological and social risk and prevention factors of eating disorders including anorexia nervosa and bulimia nervosa: seven major theories. Heliyon. 2022;8(11):e11422. doi: 10.1016/j.heliyon.2022.e11422.
- Le Grange D, O’Connor M, Hughes EK, et al. Developmental antecedents of abnormal eating attitudes and behaviors in adolescence. International Journal of Eating Disorders. 2014;47(7):813-24. doi: 10.1002/eat.22331.
- Gaudio S, Dakanalis A. Personality and eating and weight disorders: an open research challenge. Eating and Weight Disorders. 2018;23(2):143-147. doi: 10.1007/s40519-017-0463-0.
- Fassino S, Amianto F, Gramaglia C, et al. Temperament and character in eating disorders: ten years of studies. Eating and Weight Disorders. 2004;9(2):81-90. doi: 10.1007/BF03325050.
- Krug I, Root T, Bulik C, et al. Redefining phenotypes in eating disorders based on personality: a latent profile analysis. Psychiatry Research. 2011;188(3):439-45. doi: 10.1016/j.psychres.2011.05.026.
- Atiye M, Miettunen J, Raevuori-Helkamaa A. A meta-analysis of temperament in eating disorders. European Eating Disorders Review. 2015;23(2):89-99. doi: 10.1002/erv.2342.
- van Eeden AE, Hoek HW, van Hoeken D, et al. Temperament in preadolescence is associated with weight and eating pathology in young adulthood. International Journal of Eating Disorders. 2020;53(5):466-475. doi: 10.1002/eat.23241.
- Nigg JT. Temperament and developmental psychopathology. Journal of Child Psychology and Psychiatry. 2006;47(3-4):395-422. doi: 10.1111/j.1469-7610.2006.01612.x.
- Strelau J. Temperament. In: Zeigler-Hill V, Shackelford TK, editors. Encyclopedia of personality and individual differences. Springer, Cham; 2020. p. 5388-5407. doi: 10.1007/978-3-319-24612-3_446.
- Martin GC, Wertheim EH, Prior M, et al. A longitudinal study of the role of childhood temperament in the later development of eating concerns. International Journal of Eating Disorders. 2000;27(2):150-62. doi: 10.1002/(sici)1098-108x(200003)27:2<150::aid-eat3>3.0.co;2-a.
- Bufferd SJ, Levinson CA, Olino TM, et al. Temperament and psychopathology in early childhood predict body dissatisfaction and eating disorder symptoms in adolescence. Behaviour Research and Therapy. 2022;151:104039. doi: 10.1016/j.brat.2022.104039.
- Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Archives of General Psychiatry. 1993;50(12):975-90. doi: 10.1001/archpsyc.1993.01820240059008.
- Cloninger CR, Cloninger KM, Zwir I, et al. The complex genetics and biology of human temperament: a review of traditional concepts in relation to new molecular findings. Translational Psychiatry. 2019;9(1):290. doi: 10.1038/s41398-019-0621-4.
- Komasi S, Rezaei F, Hemmati A, et al. Comprehensive meta-analysis of associations between temperament and character traits in Cloninger’s psychobiological theory and mental disorders. Journal of International Medical Research. 2022;50(1):3000605211070766. doi: 10.1177/03000605211070766.
- Garcia D, Lester N, Cloninger KM, Robert Cloninger C. Temperament and character inventory (TCI). In: Zeigler-Hill V, Shackelford TK, editors. Encyclopedia of Personality and Individual Differences. Springer, Cham; 2020: p. 5408-5410. doi: 10.1007/978-3-319-24612-3_91.
- Svrakic DM, Draganic S, Hill K, et al. Temperament, character, and personality disorders: etiologic, diagnostic, treatment issues. Acta Psychiatrica Scandinavica. 2002;106(3):189-195. doi: 10.1034/j.1600-0447.2002.02196.x.
- Fassino S, Amianto F, Sobrero C, Abbate Daga G. Does it exist a personality core of mental illness? A systematic review on core psychobiological personality traits in mental disorders. Panminerva Medica. 2013;55(4):397-413.
- Garcia D, Cloninger KM, Cloninger CR. Coherence of character and temperament drives personality change toward well being in person-centered therapy. Current Opinion in Psychiatry. 2023;36(1):60-66. doi: 10.1097/YCO.0000000000000833.
- Klump KL, Bulik CM, Pollice C, et al. Temperament and character in women with anorexia nervosa. The Journal of Nervous and Mental Disease. 2000;188(9):559-67. doi: 10.1097/00005053-200009000-00001.
- Klump KL, Strober M, Bulik CM, et al. Personality characteristics of women before and after recovery from an eating disorder. Psychological Medicine. 2004;34(8):1407-18. doi: 10.1017/s0033291704002442.
- van den Bree MB, Przybeck TR, Robert Cloninger C. Diet and personality: associations in a population-based sample. Appetite. 2006;46(2):177-88. doi: 10.1016/j.appet.2005.12.004.
- Lee SJ, Cloninger CR, Chae H. Cloninger’s temperament and character traits in medical students of Korea with problem eating behaviors. Comprehensive Psychiatry. 2015;59:98-106. doi: 10.1016/j.comppsych.2015.02.006.
- Bardone-Cone AM, Wonderlich SA, Frost RO, et al. Perfectionism and eating disorders: current status and future directions. Clinical Psychology Review. 2007;27(3):384-405. doi: 10.1016/j.cpr.2006.12.005.
- Luo J, Forbush KT, Williamson JA, et al. How specific are the relationships between eating disorder behaviors and perfectionism? Eating Behaviors. 2013;14(3):291-4. doi: 10.1016/j.eatbeh.2013.04.003.
- Westwood H, Kerr-Gaffney J, Stahl D, Tchanturia K. Alexithymia in eating disorders: systematic review and meta-analyses of studies using the Toronto Alexithymia Scale. Journal of Psychosomatic Research. 2017;99:66-81. doi: 10.1016/j.jpsychores.2017.06.007.
- Wallis DJ, Ridout N. Direct and indirect effects of alexithymia on disordered eating in a non-clinical female sample: determining the role of negative affect. Frontiers in Psychiatry. 2022;13:994024. doi: 10.3389/fpsyt.2022.994024.
- Shea ME, Pritchard ME. Is self-esteem the primary predictor of disordered eating? Personality and Individual Differences. 2007;42(8):1527-1537. doi: 10.1016/j.paid.2006.10.026.
- Dakanalis A, Di Giacomo E, Colmegna F, Clerici M. Self-Esteem and Eating Disorders. In: Wade T, editor. Encyclopedia of Feeding and Eating Disorders. Springer, Singapore; 2017. p. 751-755. doi: 10.1007/978-981-287-104-6_189.
- Wagner S, Halmi KA, Maguire TV. The sense of personal ineffectiveness in patients with eating disorders: one construct or several? International Journal of Eating Disorders. 1987;6:495-505. doi: 10.1002/1098-108X(198707)6:4<495::AID-EAT2260060406>3.0.CO;2-I.
- Wade TD, Wilksch SM, Paxton SJ, et al. How perfectionism and ineffectiveness influence growth of eating disorder risk in young adolescent girls. Behaviour Research and Therapy. 2015;66:56-63. doi: 10.1016/j.brat.2015.01.007.
- Espeset EM, Gulliksen KS, Nordbø RH, et al. The link between negative emotions and eating disorder behaviour in patients with anorexia nervosa. European Eating Disorders Review. 2012;20(6):451-60. doi: 10.1002/erv.2183.
- Sahlan RN, Sala M. Eating disorder psychopathology and negative affect in Iranian college students: a network analysis. Journal of Eating Disorders. 2022;10(1):164. doi: 10.1186/s40337-022-00683-x.
- Tylka TL, Subich LM. Examining a multidimensional model of eating disorder symptomatology among college women. Journal of Counseling Psychology. 2004;51(3):314–328. doi: 10.1037/0022-0167.51.3.314.
- Juarascio AS, Perone J, Timko CA. Moderators of the relationship between body image dissatisfaction and disordered eating. Eating Disorders. 2011;19(4):346-54. doi: 10.1080/10640266.2011.584811.
- Barney JL, Barrett TS, Lensegrav-Benson T, et al. Examining a mediation model of body image-related cognitive fusion, intuitive eating, and eating disorder symptom severity in a clinical sample. Eating and Weight Disorders. 2022;27(6):2181-2192. doi: 10.1007/s40519-021-01352-9.
- Jérolon A, Perduca V, Delsedime N, et al. Mediation models of anxiety and depression between temperament and drive for thinness and body dissatisfaction in anorexia nervosa. Eating and Weight Disorders. 2022;27(7):2569-2581. doi: 10.1007/s40519-022-01397-4.
- Meshkova TA, Nikolaeva NO. Eating Attitude Test (EAT-26) on a sample of students in Moscow. Psychiatry. 2017;73:34-41. Russian.
- Meshkova TA, Mitina OV, Shelygin KV, Aleksandrova RV, Nikolaeva NO. The Eating Attitudes Test (EAT-26): psychometric characteristics and factor structure in nonclinical sample of 876 female university students. Clinical Psychology and Special Education. 2023;12(1):66–103. doi: 10.17759/cpse.2023120104. Russian.
- Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: psychometric features and clinical correlates. Psychological Medicine. 1982;12(4):871-8. doi: 10.1017/s0033291700049163.
- Maïano C, Morin AJS, Lanfranchi MC, et al. The Eating Attitudes Test-26 Revisited using exploratory structural equation modeling. Journal of Abnormal Child Psychology. 2013;41:775–788. doi: 10.1007/s10802-013-9718-z.
- McEnery F, Fitzgerald A, McNicholas F, Dooley B. Fit for purpose, psychometric assessment of the Eating attitudes test-26 in an Irish adolescent sample. Eating Behaviors. 2016;23:52-57. doi: 10.1016/j.eatbeh.2016.07.006.
- Garner DM, Olmsted MP, Polivy J. Eating Disorder Inventory. 1984;21:1009-1010.
- Bakholdina VY, Bakholdina DA, Movsesian AA, Stupina KS. On certain aspects of dembo-rubinstein method of self-esteem measurement. The Procedia - Social and Behavioral Sciences. 2014;140:547-552. doi: 10.1016/j.sbspro.2014.04.468.
- Westerberg J, Edlund B, Ghaderi A. A 2-year longitudinal study of eating attitudes, BMI, perfectionism, asceticism and family climate in adolescent girls and their parents. Eating and Weight Disorders. 2008;13(2):64-72. doi: 10.1007/BF03327605.
- Alhaj OA, Fekih-Romdhane F, Sweidan DH, et al. The prevalence and risk factors of screen-based disordered eating among university students: a global systematic review, meta-analysis, and meta- regression. Eating and Weight Disorders. 2022;27(8):3215–3243. doi: 10.1007/s40519-022-01452-0.
- Fekih-Romdhane F, Daher-Nashif S, Alhuwailah AH, et al. The prevalence of feeding and eating disorders symptomology in medical students: an updated systematic review, meta-analysis, and meta-regression. Eating and Weight Disorders. 2022;27(6):1991-2010. doi: 10.1007/s40519-021-01351-w.
- Oshio A, Meshkova T. Eating disorders, body image, and dichotomous thinking among Japanese and Russian college women. Health. 2012;4(7):392-399. doi: 10.4236/health.2012.47062.
- Costarelli V, Koretsi E, Georgitsogianni E. Health-related quality of life of Greek adolescents: the role of the Mediterranean diet. Quality of Life Research. 2013;22(5):951-6. doi: 10.1007/s11136-012-0219-2.
- Zervaki K, Yiannakouris N, Sdrali D, Costarelli V. Diet quality, disordered eating and health-related quality of life in Greek adolescents. Nutrition & Food Science. 2017;47(4):511-521. doi: 10.1108/NFS-12-2016-0189.
- Tsekoura E, Kostopoulou E, Fouzas S, et al. The association between obesity and the risk for development of eating disorders — a large-scale epidemiological study. European Review for Medical and Pharmacological Sciences. 2021;25(19):6051-6056. doi: 10.26355/eurrev_202110_26883.
- Lee AM, Lee S. Disordered eating and its psychosocial correlates among Chinese adolescent females in Hong Kong. International Journal of Eating Disorders. 1996;20(2):177-83. doi: 10.1002/(SICI)1098-108X(199609)20:2<177::AID-EAT8>3.0.CO;2-D. PMID: 8863070.
- Mak KK, Lai CM. The risks of disordered eating in Hong Kong adolescents. Eating and Weight Disorders. 2011;16(4):e289-92. doi: 10.1007/BF03327475.
- Feng T, Abebe DS. Eating behaviour disorders among adolescents in a middle school in Dongfanghong, China. Journal of Eating Disorders. 2017;5:47. doi: 10.1186/s40337-017-0175-x.
- Li S, Song L, Twayigira M, et al. Eating disorders among middle school students in a Chinese population: Prevalence and associated clinical correlates. Journal of Psychiatric Research. 2022;154:278-285. doi: 10.1016/j.jpsychires.2022.07.062.
- Fatima W, Ahmad LM. Prevalence of disordered eating attitudes among adolescent girls in Arar City, Kingdom of Saudi Arabia. Health Psychology Review. 2018;6(1):7444. doi: 10.4081/hpr.2018.7444.
- Chan MF, Al Balushi R, Al Falahi M, et al. Child and adolescent mental health disorders in the GCC: a systematic review and meta-analysis. International Journal of Pediatrics & Adolescent Medicine. 2021;8(3):134-145. doi: 10.1016/j.ijpam.2021.04.002.
- Smink FR, van Hoeken D, Oldehinkel AJ, Hoek HW. Prevalence and severity of DSM-5 eating disorders in a community cohort of adolescents. International Journal of Eating Disorders. 2014;47(6):610-9. doi: 10.1002/eat.22316.
- Kelina MY, Marenova EV, Meshkova TA. Body dissatisfaction and influence of parents and peers as risk factors for eating disorders among girls of adolescent and young age. Psychological Science and Education. 2011;16(5):44–51. Russian.
- Kelina MY, Meshkova TA. Аlexithymia and eating attitudes among adolescent and young girls of non-clinical population. Clinical Psychology and Special Education. 2012;1(2). Russian.
- Micali N, De Stavola B, Ploubidis G, et al. Adolescent eating disorder behaviours and cognitions: gender-specific effects of child, maternal and family risk factors. The British Journal of Psychiatry. 2015;207(4):320-7. doi: 10.1192/bjp.bp.114.152371.
- Nicholls D, Viner R. Eating disorders and weight problems. BMJ. 2005;330:950-953. doi: 10.1136/bmj.330.7497.950.
- Jewell T, Collyer H, Gardner T, et al. Attachment and mentalization and their association with child and adolescent eating pathology: a systematic review. International Journal of Eating Disorders. 2016;49(4):354-73. doi: 10.1002/eat.22473.
- Farstad SM, McGeown LM, von Ranson KM. Eating disorders and personality, 2004–2016: a systematic review and meta-analysis. Clinical Psychology Review. 2016;46:91-105. doi: 10.1016/j.cpr.2016.04.005.
- Aloi M, Segura-García C. Anxiety and depression mediate the role of low self-esteem and low self-directedness in the development of eating disorders. International Journal of Adolescent Medicine and Health. 2016;31(3):/j/ijamh.2019.31.issue-3/ijamh-2016-0084/ijamh-2016-0084.xml. doi: 10.1515/ijamh-2016-0084.
- Achermann M, Günther J, Goth K, et al. Body-related attitudes, personality, and identity in female adolescents with anorexia nervosa or other mental disorders. International Journal of Environmental Research and Public Health. 2022 Apr;19(7):4316. doi: 10.3390/ijerph19074316. PMID: 35409997; PMCID: PMC8998874.
- Kim SJ, Lee SJ, Yune SK, et al. The relationship between the biogenetic temperament and character and psychopathology in adolescents. Psychopathology. 2006;39(2):80-6. doi: 10.1159/000090597.
- van der Heijden PT, Egger JI, Rossi GM, et al. Personality and psychopathology: mapping the MMPI-2-RF on Cloninger’s psychobiological model of personality. Assessment. 2013;20(5):576-84. doi: 10.1177/1073191113490791.
- Krug I, King RM, Youssef GJ, et al. The effect of low parental warmth and low monitoring on disordered eating in mid-adolescence: findings from the Australian Temperament Project. Appetite. 2016;105:232-41. doi: 10.1016/j.appet.2016.05.015. PMID: 27212673.
- Laghi F, McPhie ML, Baumgartner E, et al. Family functioning and dysfunctional eating among Italian adolescents: the moderating role of gender. Child Psychiatry & Human Development. 2016;47(1):43-52. doi: 10.1007/s10578-015-0543-1.
- Westerberg-Jacobson J, Edlund B, Ghaderi A. Risk and protective factors for disturbed eating: a 7-year longitudinal study of eating attitudes and psychological factors in adolescent girls and their parents. Eating and Weight Disorders. 2010;15(4):e208-18. doi: 10.1007/BF03325302.
- Teixeira MD, Pereira AT, Marques MV, et al. Eating behaviors, body image, perfectionism, and self-esteem in a sample of Portuguese girls. Brazilian Journal of Psychiatry. 2016;38(2):135-40. doi: 10.1590/1516-4446-2015-1723.
- Mustapic J, Marcinko D, Vargek P. Eating behaviours in adolescent girls: the role of body shame and body dissatisfaction. Eating and Weight Disorders. 2015;20(3):329-35. doi: 10.1007/s40519-015-0183-2.
- Schmitt AP, Hart E, Chow CM. Attachment, rumination, and disordered eating among adolescent girls: the moderating role of stress. Eating and Weight Disorders. 2021;26(7):2271-2279. doi: 10.1007/s40519-020-01029-9.
- Bacopoulou F, Foskolos E, Stefanaki C, et al. Disordered eating attitudes and emotional/behavioral adjustment in Greek adolescents. Eating and Weight Disorders. 2018;23(5):621-628. doi: 10.1007/s40519-017-0466-x.
- Pace U, D’Urso G, Zappulla C. Negative eating attitudes and behaviors among adolescents: the role of parental control and perceived peer support. Appetite. 2018;121:77-82. doi: 10.1016/j.appet.2017.11.001.
- Chardon ML, Janicke DM, Carmody JK, Dumont-Driscoll MC. Youth internalizing symptoms, sleep-related problems, and disordered eating attitudes and behaviors: a moderated mediation analysis. Eating Behaviors. 2016;21:99-103. doi: 10.1016/j.eatbeh.2016.01.007.
- Mohorić T, Pokrajac-Bulian A, Anić P, et al. Emotion regulation, perfectionism, and eating disorder symptoms in adolescents: the mediating role of cognitive eating patterns. Current Psychology. 2022:1-12. doi: 10.1007/s12144-022-03824-2.
- Jones H, McIntosh VVW, Britt E, et al. The effect of temperament and character on body dissatisfaction in women with bulimia nervosa: the role of low self-esteem and depression European Eating Disorders Review. 2022;30(4):388-400. doi: 10.1002/erv.2899.
- Wolz I, Agüera Z, Granero R, et al. Emotion regulation in disordered eating: psychometric properties of the Difficulties in Emotion Regulation Scale among Spanish adults and its interrelations with personality and clinical severity. Frontiers in Psychology. 2015;6:907. doi: 10.3389/fpsyg.2015.00907.
- Paganini C, Peterson G, Andrews K. The mediating role of temperamental traits on the relationship between age of puberty and eating disorders: a mediating analysis through structural equation modelling of Australian eating disorder outpatients. The Journal of Genetic Psychology. 2021;182(6):391-405. doi: 10.1080/00221325.2021.1940822.
- Monteleone AM, Cascino G. A systematic review of network analysis studies in eating disorders: is time to broaden the core psychopathology to non specific symptoms. European Eating Disorders Review. 2021;29(4):531-547. doi: 10.1002/erv.2834.
- Punzi C, Petti M, Tieri P. Network-based methods for psychometric data of eating disorders: a systematic review. PLoS ONE. 2022;17(10):e0276341. doi: 10.1371/journal.pone.0276341.
- Vervaet M, Puttevils L, Hoekstra RHA, et al. Transdiagnostic vulnerability factors in eating disorders: A network analysis. European Eating Disorders Review. 2021;29(1):86-100. doi: 10.1002/erv.2805.
Information About the Authors
Metrics
Web Views
Whole time: 548
Previous month: 43
Current month: 22
PDF Downloads
Whole time: 231
Previous month: 22
Current month: 12
Total
Whole time: 779
Previous month: 65
Current month: 34