Consortium Psychiatricum
2022. Vol. 3, no. 3, 58–72
doi:10.17816/CP172
ISSN: 2712-7672 / 2713-2919 (online)
Clinical Effectiveness of Lurasidone Monotherapy in Patients with Acute Episodes of Schizophrenia and Associated Symptoms of Depression*
Abstract
AIM: We endeavored to evaluate the efficacy of Lurasidone at doses of 40–160 mg per day on symptoms of schizophrenia associated with symptoms of depression in real clinical practice in a Russian patient population.
METHODS: One hundred sixty eight patients aged 18–65 years old, who at the time of the start of the observation were being treated in a hospital or day hospital due to an exacerbation of paranoid schizophrenia accompanied by symptoms of depression, were prescribed lurasidone. Treatment with lurasidone and other concomitant drugs, their prescription, withdrawal, selection, and dose modifications were determined based on the indications for the use of those drugs and the recommended doses in the instructions, clinical need, and patient interests, rather than by the goals of the study. During the observation period, the severity of depressive symptoms according to the Calgary Depression Scale (CDSS) and that of psychotic symptoms according to the Positive and Negative Syndrome Scale (PANSS) were assessed six times (before the start of treatment and then on the 4th, 7th, 14th, 28th, and 42nd days).
RESULTS: A statistically significant reduction in the severity of the symptoms was observed with the use of lurasidone in doses ranging from 40 mg to 160 mg per day. The fastest and most significant (p <0.001) reductions in the total PANSS and CDSS scores were observed with lurasidone 120 mg. A somewhat lower efficacy of lurasidone was observed at a dose of 160 mg. The largest reductions in the total PANSS and CDSS scores with lurasidone 120 mg were associated with the highest survival rate and the longest median time from treatment initiation to discontinuation or follow-up. The most commonly reported side effects with lurasidone in this study (nausea, akathisia, tremor and drowsiness) were consistent with the known safety profile of the drug. Adverse events in most cases were assessed as mild, or occasionally moderate.
CONCLUSION: A six-week prospective observational study of the real-world clinical effectiveness of lurasidone in doses ranging from 40 mg to 160 mg per day established statistically and clinically significant improvements in both psychotic and depressive symptoms in patients with acute exacerbation of schizophrenia and associated symptoms of depression.
General Information
* The data presented in this publication are a part of the Molecular and Neurophysiological Markers of Endogenous Diseases Research Program, conducted at the SBHI Psychiatric Clinical Hospital No.1 of the Moscow Healthcare Department and approved by the Independent Interdisciplinary Ethics Committee on Ethical Review for Clinical Studies on July 14, 2017 (protocol No. 12).
Keywords: lurasidone, schizophrenia, depression, exacerbation of schizophrenia, second-generation antipsychotic, psychopharmacotherapy
Journal rubric: Researches
Article type: scientific article
DOI: https://doi.org/10.17816/CP172
Funding. The observational study was sponsored by OAO Angelini Pharma Rus (open joint-stock company). The authors developed the study design, data collection and analysis, and interpretation of the results. The authors independently decided to publish this study in the journal Consortium Psychiatricum.
Received: 30.03.2022
Accepted:
For citation: Reznik A.M., Syunyakov T.S., Akhmerova I.Yu., Butylin D.Yu., Vasilenko A.O., Gvozdetckii A.N., Gizatullin T.R., Gilmanshina G.V., Golosov E.A., Kolchev S.A., Linova L.P., Miron D.V., Mudrak A.V., Oleichik I., Sizov S.V., Tarakanova E.A., Chesnokova O.I. Clinical Effectiveness of Lurasidone Monotherapy in Patients with Acute Episodes of Schizophrenia and Associated Symptoms of Depression. Consortium Psychiatricum, 2022. Vol. 3, no. 3, pp. 58–72. DOI: 10.17816/CP172.
Full text
INTRODUCTION
A significant number of patients with schizophrenia experience symptoms of depression [1–5]. Depression has been observed in 20% of patients with schizophrenia during remission, while its incidence increases to 60% during acute episodes. The incidence of depression can reach 80% based on medical history, particularly in the early stages of schizophrenia [6]. Depression is one of the main symptoms of schizophrenia and one of the diagnostic signs of schizophrenia spectrum disorders [5–7]. This does not contradict the traditional division drawn between affective disorders and schizophrenia. An intermediate diagnostic category of schizoaffective psychosis defines the concept of phenotypes with a different representation of psychotic and affective disorders, or a multidimensional phenomenological continuum from conditionally “pure” schizophrenia to “pure” bipolar disorder [8–10]. The remaining challenge is determining the key features that allow one to distinguish between intermediate forms of psychotic and affective disorders. For example, symptoms of depression in patients with schizophrenia are associated with cognitive impairment. These symptoms are difficult to distinguish from the typical negative symptoms of schizophrenia in real-world clinical practice. Differential diagnosis is difficult, because signs of irreversible negative symptoms are similar to signs of depression, even in definite and long-term schizophrenia [1, 5, 11, 12]. Difficulties in the differential diagnosis between affective disorders or negative symptoms are common in the presence of symptoms such as anhedonia, mental anesthesia, emotional indifference, loss of motivation, anergy, flat affect, social withdrawal, ideational retardation, and impoverished thinking [1, 6, 11, 13]. Sometimes it is difficult to immediately distinguish between depression and catatonia [14, 15]. Notably, severe depression might be associated with psychotic features, such as delusions, hallucinations, and conceptual disorganization [1]. Sometimes, symptoms of depression are obvious signs of established schizophrenia. Even in such cases, there is the problem of determining the role of depression in the structure of the psychopathological syndrome, determining its influence on the course of the disease, its role as a target of therapy, and the complications [13, 16]. Treatment for depression associated with schizophrenia usually includes various combinations of antipsychotics, mood stabilizers, and antidepressants. However, this approach is controversial and associated with polypharmacy [13, 16–22]. This combined treatment has both desirable and adverse effects [19, 22]. The combination and severity of both affective and psychotic symptoms in a patient with schizophrenia should inform the selection of pharmacological treatment. An ideal treatment should affect depressive, positive, and negative symptoms, and it should carry minimal risk of complications. Drugs that combine the properties of antipsychotics and antidepressants due to the polyvalence of neurochemical activity appear promising [4, 13, 21, 23]. Lurasidone (Latuda®) demonstrates such properties, and it possesses selectivity for and high affinity to dopamine D2 receptors [24–26], partial agonism to 5-HT1А, antagonism to 5-HT2А, and antagonism to the 5-HT7 subtype of serotonin receptors [24, 27]. It also demonstrates selective antagonism to the α2С subtype adrenergic receptors in the prefrontal cortex [27]. Strong selective D2 receptor antagonism provides a reliable antipsychotic effect with minimal involvement of dopamine transmission in the prefrontal cortex and associated minimal effects on cognitive functions, while a complex effect on the serotonergic system provides much more diverse clinical effects of the drug. Thus, partial agonism to 5-HT1А and blockade of 5-HT2А increase the dopamine level in the prefrontal cortex and reduce the cognitive and negative impairments associated with schizophrenia. Lurasidone also normalizes the dopamine levels in the nigrostriatal and tuberoinfundibular pathways, which reduces the risk of extrapyramidal symptoms and neuroleptic depression [25, 28]. The incidence of hyperprolactinemia was comparable to the placebo [29]. Due to the blockade of 5-HT7 receptors, lurasidone possesses antidepressant and anxiolytic properties, normalizes circadian rhythms and sleep quality, improves memory, concentration, and cognition, reduces pain sensitivity, and even possesses an antipsychotic effect [27, 28]. Lurasidone increases the release of norepinephrine and, thereby, contributes to its antidepressant effect by blocking presynaptic and autoregulatory α2С adrenergic receptors [27]. At the same time, it has no appreciable affinity for the M cholinergic, α1 adrenergic, 5-HT2С serotonin, or histamine H1 receptors, which are “undesirable” receptor targets. Thus, lurasidone rarely causes such adverse events as paresis of accommodation, urinary retention, cognitive and memory impairment, tachycardia and orthostatic hypotension, QT prolongation, metabolic disorders, drowsiness, increased appetite, and weight gain [24, 25, 27–29]. Moreover, patients previously treated with some other second-generation antipsychotics have experienced weight loss within a year of switching to lurasidone therapy [30, 31]. In general, a positive impact on body weight, metabolism, and prolactin levels has been noted after a switch to lurasidone. It possesses a very low probability of drug-drug interaction [32]. Lurasidone is overall well-tolerated by patients, and it could be used in the presence of various comorbid mental conditions. Lurasidone has been established as a drug of choice in patients with metabolic disorders and cardiovascular risks [32].
Lurasidone is effective in the treatment of acute psychotic symptoms, as has been demonstrated by a number of RCTs. Its efficacy is similar to that of other second-generation antipsychotics [29, 33–36]. Lurasidone robustly reduces the scores of Marder PANSS factors [37] of positive symptoms and arousal/aggression. At the same time, significant improvement is also evident on all other PANSS parameters, including anxiety/depression, as well as cognitive impairment/disorganization [38]. While on lurasidone, patients have reported greater awareness of their illness and have been more compliant with treatment [39]. The effectiveness of the drug at reducing symptoms of depression was also confirmed using MADRS [35] and HDRS-21 [40]. Lurasidone has demonstrated a long-term relapse-prevention antidepressant effect [36]. Patients taking lurasidone have a higher level of compliance and lower discontinuation rates compared to patients taking other atypical antipsychotics [32, 41]. Lurasidone has demonstrated efficacy in acute bipolar depression, both as monotherapy [42] and in combination with mood stabilizers [43]. Studies showed relief of depression and anxiety, as well as cognitive and quality-of-life improvement. It is important that the incidence of affective phase inversion of bipolar disorder was the same as with the placebo. Therefore, lurasidone presents valuable treatment options for bipolar disorder [42, 43]. Lurasidone proved superior to placebo in terms of the effects on depressive symptoms during the acute phase of schizophrenia according to the pooled RCT analysis. Moreover, the antidepressant effect does not depend on the antipsychotic effect [35, 40, 44]. The data support the inclusion of lurasidone in the treatment of depressive symptoms in patients with schizophrenia [44]. Thus, lurasidone possesses a wide range of non-dopamine receptor activities, which determine its antidepressant and pro-cognitive effect, along with its impact on negative symptoms. Lurasidone represents an alternative to routine treatment where patients with schizophrenia and depressive symptoms are given an antipsychotic along with an antidepressant. However, the effectiveness of lurasidone in exacerbations of schizophrenia, including psychotic and depressive symptoms in a real-world setting, requires additional research.
The objective of this study was to evaluate the effectiveness of lurasidone 40–160 mg per day for the treatment of an acute episode of schizophrenia associated with depressive symptoms in real-world clinical practice in the Russian patient population.
The objectives of the observational program included:
- assessing symptoms of schizophrenia using the Positive and Negative Syndrome Scale (PANSS);
- assessing depressive symptoms using the Calgary Depression Symptoms Scale (CDSS); and
- evaluating lurasidone safety and tolerability.
The primary endpoint was to achieve a decrease in depressive symptoms consistent with the Minimum Clinically Important Difference (MCID), characterized by a decline of at least 1.3 points according to the CDSS [45]. A secondary endpoint was a reduction in the severity of schizophrenia symptoms, as measured by PANSS and its subscales (positive and negative symptoms and general psychopathology).
METHODS
Study design
A prospective observational cohort study of patients with acute exacerbation of schizophrenia, concomitant with depressive symptoms, was conducted in Russian specialized research institutes and health care facilities: Mental Health Research Center and Psychiatric Hospital No. 1 named after N.A. Alexeev (Moscow), Psychiatric Hospital No. 1 named after P.P. Kashchenko, City Psychiatric Hospital No. 3 named after I.I. Skvortsov-Stepanov and City Psychiatric Hospital No. 6 (St. Petersburg), Republican Clinical Psychiatric Hospital, Republic of Bashkortostan (Ufa), Stavropol Regional Clinical Psychiatric Hospital No. 1 (Stavropol), and the Volgograd Regional Psychiatric Hospital (Volgograd). The study sample consisted of men and women with confirmed diagnoses of schizophrenia (per DSM-V-TR) and concomitant depressive symptoms who were prescribed lurasidone at a dose of 40–160 mg per day.
Inclusion criteria:
- written informed consent for the collection and anonymized processing of socio-demographic, medical, and psychometric data;
- paranoid schizophrenia (F20) diagnosed according to ICD-10, including F20.00 — continuous course; F20.01 — episodic course with a progressive defect; F20.02 — episodic course with a stable defect; F20.03 — episodic relapsing (recurrent) current F20.09 — follow-up period of less than a year;
- schizophrenia exacerbation which required a change in a health care setting (treatment in psychiatric hospital or outpatient hospital), changes in antipsychotic therapy, and second-generation antipsychotics prescription; exacerbation included psychotic symptoms and the onset or worsening of depressive symptoms requiring pharmacological intervention as judged by the treating physician;
- moderate or severe exacerbation: a total PANSS score of at least 70 and a total CDSS score of at least 6;
- lurasidone prescription (treating physician prescribes lurasidone regardless of the program design and the objective of the study); and
- aged between 18 and 65 years old.
Exclusion criteria:
- refusal or lack of capacity to comply with study evaluation;
- participation in another clinical study;
- lurasidone contraindications which were determined by the physician according to the clinical signs of the disease, concomitant diseases, and other individual risks, as well as contraindications specified in the instructions for use approved by the Ministry of Health of the Russian Federation.
All patients received lurasidone orally once or twice daily as clinically appropriate and indicated by current clinical guidelines in the Russian Federation. The primary treating physicians determined the treatment regimen based on the individual needs of each patient; the physicians were not influenced by the objectives of the study. Patients could receive concomitant medications (i.e., mood stabilizers, sedatives, hypnotics, etc.) as clinically indicated.
Premature cessation of follow-up occurred after discontinuation of lurasidone for any reason, such as when the physician changed the antipsychotic or prescribed a second antipsychotic with a strong selective antipsychotic effect, when lurasidone was not effective against depressive symptoms and an antidepressant had to be prescribed, or when the physician or patient had decided to discontinue follow-up in the best interests of the patient.
The study was conducted from December 2020 to September 2021. Study evaluations were done before the start of treatment, on Day 1 and then on Days 4, 7, 14, 28, and 42 with an allowable interval of ±1 day. The maximum follow-up period for each patient was six weeks. We developed a special individual registration card that included anonymous data on the age, locality, diagnosis, additional therapies, the presence or absence of adverse events, and predominant symptoms and their severity. We recorded the onset, completion, or discontinuation of the study, indicating the reasons for the latter.
Evaluation tools
Psychotic and depressive symptoms were quantified using special scales, such as:
1) The Calgary Depression Scale for Schizophrenia (CDSS) [46], which is a nine-item scale where each item is scored from 0 to 3. The scale showed high internal and interrater reliability in assessing the depressive symptoms associated with schizophrenia [46].
2) Positive and Negative Syndrome Scale (PANSS), which typologically and multidimensionally evaluates psychopathological symptoms [47].
The study group included 168 patients aged 18 to 65 with a diagnosis of paranoid schizophrenia according to ICD-10. All of them were treated in an inpatient facility or day hospital for schizophrenia exacerbation, accompanied by depressive symptoms at the time of the study onset. One hundred forty one patients (83.9%) completed the observational program and made seven visits.
Statistical analysis
The general characteristics of the population are processed using descriptive statistics. Continuous variables are presented as mean values, standard deviations (SD), medians, and first and third quartiles (Q1 and Q3). Qualitative variables are presented as frequencies and percentages. Mean values were compared between the groups using a one-way analysis of variance (One-way ANOVA), and the distribution of categorical variables using Fisher’s exact test. Data were analyzed according to the PANSS positive (P1–P7), negative symptoms (N1–N7), and general psychopathology (G1–G16) subscale scores, PANSS total score, CDSS total score, and time to study completion. The significance of score changes on the scales was assessed via a dispersion analysis for repeated measurements (single-factor or multi-factor, depending on the comparison type). We also assessed changes in scale scores during each visit between groups. The study calculated the differences between Visit 1 and Visit n, which were then entered into a two-way ANOVA to compare groups. Post-hoc comparisons took into account the appropriate correction for multiple comparisons according to Dunnett’s test for duplicate values and Tukey’s test for between-group contrasts, when necessary.
We calculated the average and total doses of lurasidone for each patient and then determined the total drug exposure and the individual dose range (40–80, 120, or 160 mg per day).
Time to study completion was evaluated using the Kaplan-Meier survival analysis.
All analyses were performed using the GraphPad software (GraphPad Prism version 9.3.1 for Windows, GraphPad Software, San Diego, California USA, www.graphpad.com), except for the survival analysis, which was done using the NCSS software (NCSS 2021 Statistical Software (2021). NCSS, LLC. Kaysville, Utah, USA, ncss.com/software/ncss.)
The analysis included all patients, even those who dropped out of the study prematurely. The last-observation-carried-forward (LOCF) approach was used for the patients who dropped out of the study prematurely.
RESULTS
All study patients displayed various forms of paranoid schizophrenia at the start of the treatment for their then-exacerbation in a psychiatric hospital. The mean age of the men and women did not differ significantly. The main psychopathological syndromes at the start of the follow-up were affective-delusional, including depressive-paranoid (n=95), hallucinatory-paranoid (n=44), depressive or anxious-depressive (n=28), and catatonic (n=1). All patients experienced depressive symptoms of varying severities.
Table 1 shows descriptive sample statistics.
Table 1. Clinical and demographic characteristics of the studied group of patients
|
Gender |
Females (N=112) |
Males (N=56) |
Total (N=168) |
Test statistics |
|
Age 1 |
F=0.095, df=1, p=0.758 |
|||
|
Mean (SD) |
31.667 (11.168) |
31.125 (9.701) |
31.485 (10.672) |
|
|
Median (Q1, Q3) |
30 (23, 37) |
31 (25, 38.25) |
31 (23, 37.5) |
|
|
First psychotic episode 2 |
p=0.032 |
|||
|
No |
58 (51.8%) |
33 (58.9%) |
91 (54.2%) |
|
|
Yes |
19 (17.0%) |
3 (5.4%) |
22 (13.1%) |
|
|
Missed |
35 (31.2%) |
20 (35.7%) |
55 (32.7%) |
|
|
Age of first psychotic episode 1 |
F=3.831, df=1, p=0.053 |
|||
|
Missed |
35 |
20 |
55 |
|
|
Mean (SD) |
18.260 (12.444) |
22.750 (8.554) |
19.690 (11.505) |
|
|
Median (Q1, Q3) |
20 (15, 24) |
21.5 (18.75, 26.25) |
20 (18, 25) |
|
|
Hospitalization Number 1 |
F=4.235, df=1, p=0.041 |
|||
|
Missed |
2 |
1 |
3 |
|
|
Mean (SD) |
2.600 (1.978) |
3.327 (2.435) |
2.842 (2.161) |
|
|
Median (Q1, Q3) |
2 (1, 3) |
3 (2, 4) |
2 (1, 4) |
|
Note: 1 One-way ANOVA, 2 Fisher exact test. Statistical test are provided for non-missed comparisons between males and females.
Primary and secondary lurasidone effectiveness endpoints
The primary lurasidone effectiveness endpoint in the study was the comparison of the changes in the total CDSS score over the study period. Secondary endpoints were the changes in the total PANSS and positive, negative, and general psychopathology subscale scores in the comparison. Table 2 shows the ANOVA results for repeated measurement of the evaluation parameters; the independent factor is the visit number. Table 3 and Figure 1 show details of the means compared to Visit 1 according to a post-hoc analysis with Dunnett’s test correction. All effectiveness parameters demonstrated a significant visit effect, according to partial eta-squared values ranging from 0.39 to 0.59, reflecting the large impact of size (CDSS ηp2=0.48, PANSS, positive subscale ηp2=0.55, PANSS, negative subscale ηp2=0.53, PANSS, general psychopathology subscale ηp2=0.39, PANSS total score ηp2=0.59) (Table 2). The mean (95% CI) reduction in the total CDSS score at Visit 5 compared to Visit 1 was 7.000 [5.72–8.28] points (t(167)=13.49, p <0.001). Mean changes in the positive, negative, and general psychopathology subscales, as well as the total PANSS score, were 9.02 [7.61–10.44] (t(167)=15.74, p <0.001), 7.98 [6.62–9.33] (t(167)=14.54, p <0.001), 1.77 [14.00–22.71] (t(167)=10.40, p <0.001) and 38.14 [32.32–43.95] (t(167)=16.16, p <0.001), respectively (Table 3). Each effectiveness parameter at Visit 1 showed statistical differences starting from Visit 2.
Figure 1. Changes in the total PANSS and CDSS scores.
Table 2. Primary (CDSS total score) and secondary (PANSS positive subscale, negative subscale, general psychopathology subscale, PANSS total score) outcome variables for Repeated Measures ANOVA Results
|
Scale / subscale |
df |
Sum of Squares |
Mean Square |
F |
F (DFn, DFd) |
p |
ηp2 |
|
CDSS total score |
4 |
6324.73 |
1581.18 |
154.36 |
F (1,463, 244,3)=156,7 |
<0.001 |
0.48 |
|
PANSS, positive subscale |
4 |
8672.64 |
2168.16 |
200.88 |
F (1,491, 249,0)=195,5 |
<0.001 |
0.55 |
|
PANSS, negative subscale |
4 |
6728.98 |
1682.25 |
185.99 |
F (1,582, 264,2)=171,9 |
<0.001 |
0.53 |
|
PANSS, general psychopathology subscale |
4 |
37098.85 |
9274.71 |
107.56 |
F (1,593, 266,0)=103,7 |
<0.001 |
0.39 |
|
PANSS total score |
4 |
150164.85 |
37541.21 |
242.39 |
F (1,455, 243,0)=218,6 |
<0.001 |
0.59 |
Table 3. Primary (CDSS total score) and secondary (PANSS positive subscale, negative subscale, general psychopathology subscale, PANSS total score) outcome variables means and mean changes from the background (repeated-measures ANOVA, LOCF)
|
Variable |
Day |
Mean |
S.D. |
CI 95% of the mean |
Mean change |
CI 95% of the mean change |
t |
df |
Dunnett’s p |
|
CDSS total score |
1 |
16.81 |
7.19 |
15.71–17.91 |
|||||
|
7 |
14.51 |
6.95 |
13.45–15.57 |
2.304 |
1.58–3.02 |
7.883 |
167 |
<0.001 |
|
|
14 |
10.75 |
6.46 |
9.76–11.74 |
6.060 |
4.95–7.17 |
13.42 |
167 |
<0.001 |
|
|
28 |
10.19 |
6.49 |
9.19–11.18 |
6.625 |
5.43–7.82 |
13.62 |
167 |
<0.001 |
|
|
42 |
9.81 |
6.65 |
8.79–10.83 |
7.000 |
5.72–8.28 |
13.49 |
167 |
<0.001 |
|
|
PANSS Positive Subscale score |
1 |
22.11 |
5.20 |
21.31–22.90 |
|||||
|
7 |
19.69 |
5.25 |
18.89–20.49 |
2.42 |
1.76–3.08 |
9.03 |
167 |
<0.001 |
|
|
14 |
16.96 |
5.58 |
16.11–17.82 |
5.14 |
4.12–6.16 |
12.45 |
167 |
<0.001 |
|
|
28 |
14.76 |
5.92 |
13.85–15.66 |
7.35 |
6.11–8.60 |
14.57 |
167 |
<0.001 |
|
|
42 |
13.08 |
6.34 |
12.12–14.05 |
9.02 |
7.61–10.44 |
15.74 |
167 |
<0.001 |
|
|
PANSS Negative Subscale score |
1 |
26.65 |
5.60 |
25.79–27.50 |
|||||
|
7 |
24.54 |
5.19 |
23.75–25.34 |
2.11 |
1.40–2.82 |
7.34 |
167 |
<0.001 |
|
|
14 |
22.33 |
5.08 |
21.55–23.10 |
4.32 |
3.41–5.24 |
11.66 |
167 |
<0.001 |
|
|
28 |
20.09 |
5.45 |
19.26–20.92 |
6.56 |
5.40–7.72 |
13.90 |
167 |
<0.001 |
|
|
42 |
18.67 |
6.02 |
17.75–19.59 |
7.98 |
6.62–9.33 |
14.54 |
167 |
<0.001 |
|
|
1 |
55.60 |
12.72 |
53.65–57.54 |
||||||
|
7 |
49.42 |
10.18 |
47.87–50.98 |
0.71 |
4.41–7.93 |
8.65 |
167 |
<0.001 |
|
|
14 |
43.98 |
9.63 |
42.51–45.45 |
0.96 |
9.25–14.00 |
12.11 |
167 |
<0.001 |
|
|
28 |
38.71 |
10.54 |
37.10–40.32 |
1.16 |
14.02–19.76 |
14.51 |
167 |
<0.001 |
|
|
PANSS General psychopathology Subscale score |
42 |
37.24 |
16.01 |
34.79–39.68 |
1.77 |
14.00–22.71 |
10.40 |
167 |
<0.001 |
|
PANSS total score |
1 |
104.35 |
20.12 |
101.28–107.42 |
|||||
|
7 |
93.61 |
17.55 |
90.93–96.30 |
10.74 |
7.71–13.77 |
8.74 |
167 |
<0.001 |
|
|
14 |
83.23 |
17.90 |
80.50–85.97 |
21.12 |
17.02–25.22 |
12.71 |
167 |
<0.001 |
|
|
28 |
73.49 |
20.17 |
70.41–76.57 |
30.86 |
25.83–35.90 |
15.10 |
167 |
<0.001 |
|
|
42 |
66.21 |
23.12 |
62.68–69.75 |
38.14 |
32.32–43.95 |
16.16 |
167 |
<0.001 |
We assessed the rate of symptom reduction according to the PANSS and CDSS and found a significant difference in favor of depressive symptom reduction by Week 2.
Correlation between the mean dose of lurasidone and the mental status
Some 13 (8%) patients took the drug at a dose of 40 to 80 mg, 87 patients (53.7%) — over 80 mg and up to 120 mg; and 62 (38.3 %) — over 120 mg and up to 160 mg. Repeated measures ANOVA showed no significant interaction effect between the lurasidone dose and treatment duration on the total CDSS score (F (8,660)=1.383, p=0.200).
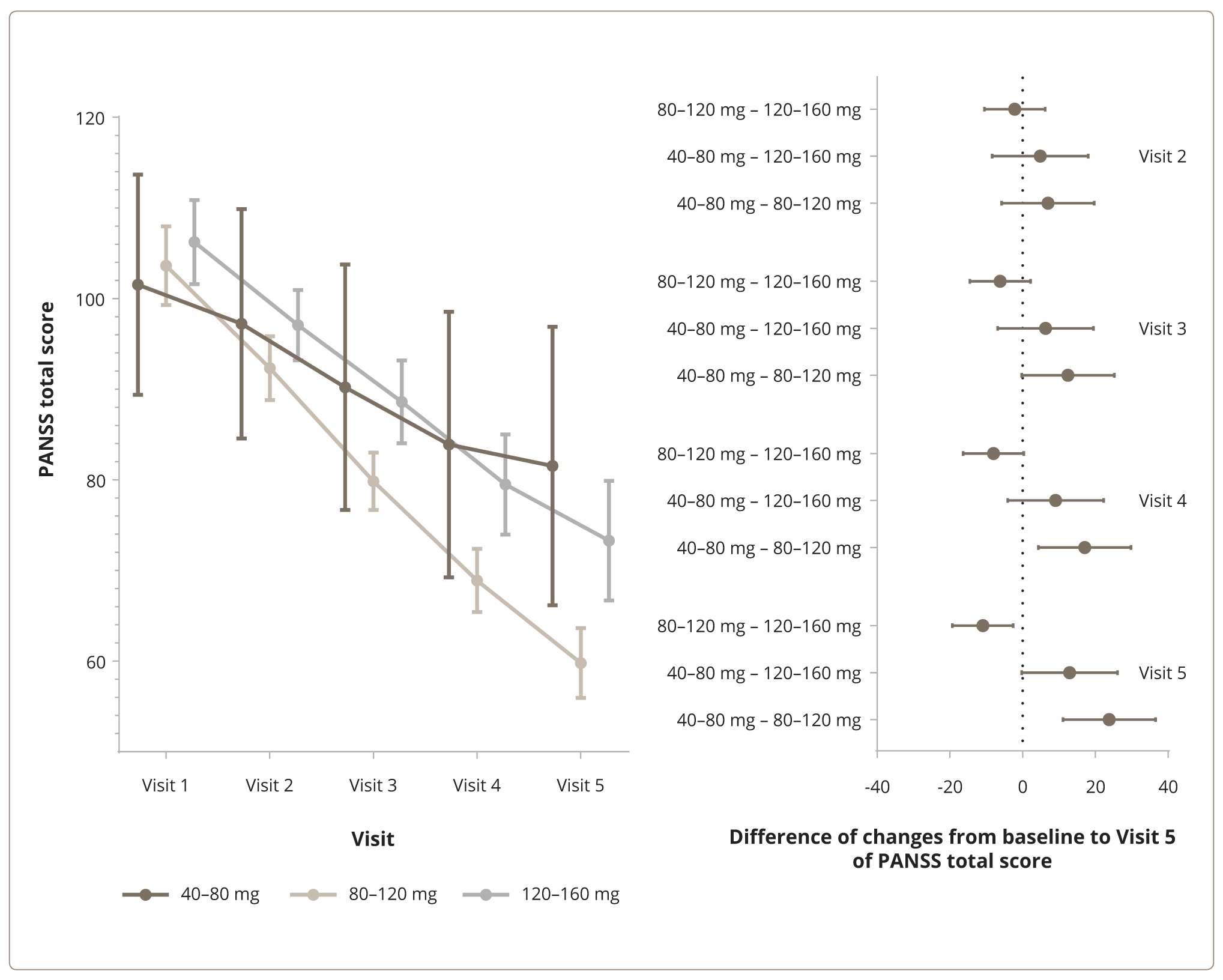
Assessment of the total PANSS score revealed a statistical interaction between the average lurasidone dose and the treatment duration (F(8, 660)=5.479, p <0.001, ηp2=0.06). Figure 2 shows the changes and mean differences in the PANSS total score compared to Visit 1, depending on the dosage. A pairwise comparison of the changes in baseline values at Visit 5 revealed significant differences between doses of over 80 mg and up to 120 mg per day, doses from 40 to 80 mg per day, and over 120 to 160 mg per day (mean difference [95% CI]: 23.85 [11.12, 36.58], t=4.484, p <0.001 and 10.92 [2.56, 19.27], t=3.127, p=0.006, respectively). Doses over 80 mg and up to 120 mg per day were found to be superior.
Figure 2. Changes in the total score (left) and mean differences compared to Visit 1 (right) according to the PANSS and the average daily doses of lurasidone: from 40 mg to 80 mg, over 80 and up to 120 mg, and over 120 mg and up to 160 mg.
Twenty-seven patients completed the study ahead of schedule. Among them, five patients (38.5% of all the patients taking lurasidone in this dose range) took the drug at a daily dose of 40–80 mg, eight (9.2%) patients at 80–120 mg, and 14 (22.6%) patients at 120–160 mg. The median [95% CI] duration of participation was 31.79 [21.328–42.244], 60.48 [57.248–63.710], and 52.26 [46.613–57.903] among patients taking lurasidone at a dose of 40–80 mg per day, 80–120 mg per day, and 120–160 mg per day, respectively. Figure 3 shows the results of a Kaplan-Meier survival analysis among patients treated with lurasidone at daily doses of 40–80 mg, 80–120 mg, and 120–160 mg, respectively. A dose range of 80–120 mg was associated with a statistically longer use of lurasidone compared to the dose ranges (i.e., 40–80 mg) (Restricted Mean Survival Time (RMST) Difference [95% CI]: 20 [4–37] days, z=1.488, p=0.01) and 120–160 mg (mean [95% CI] difference: 8 [1–14] days, z=2.31, p=0.02).
Figure 3. The Kaplan-Meier survival analysis of dosage: from 40 mg to 80 mg, over 80 mg and up to 120 mg, and over 120 mg and up to 160 mg.
Tolerability analysis
Total lurasidone exposure was 657,120 mg, and the total treatment duration was 6,207 person-days.
The study recorded 143 adverse events (AEs) among 85 patients. A complete list of the AEs is given in the Appendix. The most common (in >5% of patients) AEs were: akathisia, in 22 patients (13%); nausea, in 19 patients (11%); tremor, in 14 patients (8%); drowsiness, in 12 patients (7%); headache, in 11 patients (7%); and sleep disruption, in 8 patients (5%). Among 143 AEs, 71 (49.7%) were mild; 60 (42.0%), moderate; and 12 (8.4%), severe. Ten cases of AEs led to premature study termination: two cases of acute dystonia, two cases of tremor, two cases of night sleep disturbance, increased drowsiness, akathisia, pneumonia, and seizures. Overall, the majority of AEs (131 (91.6%) cases) occurred within the first week of therapy, with 22 (17.8%) cases lasting more than one week.
We found a correlation between the mean number of AEs and the average daily dose (F=3.41, p=0.035, one-way ANOVA). The mean daily dose of 40–80 mg corresponded to 0.37 AEs, 80–120 mg per day corresponded to 0.8 AEs, and 120–160 mg per day corresponded to 1.06 AEs. A pairwise post-hoc analysis uncovered statistical differences in mean AE rates between the 40–80 mg per day and 120–160 mg per day dose ranges (mean difference 0.7 [0.03–1.37], t=2.54, p=0.012). A table of the AE incidence and average daily dose is given in the Appendix.
DISCUSSION
This short-duration prospective observational study of the effectiveness of lurasidone in a dose ranging from 40 mg to 160 mg per day has established statistically and clinically significant improvement in both psychotic and depressive symptoms for patients with acute exacerbation of schizophrenia and depressive symptoms. Significant reductions in the PANSS and CDSS scores were noted at all lurasidone dosages (from 40 mg to 160 mg daily) starting with Week 1 of the follow-up period. There is extensive data on lurasidone effectiveness in a situation of acute exacerbations and long-term maintenance of schizophrenia [25, 36, 38, 41], as well as in the treatment of depression [35, 40, 44]. The antipsychotic activity of the drug established in this study was comparable to the results achieved in short-term randomized controlled trials (RCTs) [36, 38]. This study demonstrated the reality of a statistical reduction in the severity of psychotic and depressive symptoms for patients treated with lurasidone at doses of 40 mg to 160 mg per day. However, lurasidone at a daily dose of 120 mg reduced the total PANSS score considerably more than at doses of 40 mg to 80 mg, and over 120 mg (mean difference 23.85 [11.12, 36.58], t=4.484, p <0.001 and 10.92 [2.56, 19.27], t=3.127, p=0.006, respectively). In our opinion, the lower effectiveness of lurasidone at a dose of 160 mg in this study has to do with potential resistance to the treatment among those who were advanced to that dose after insufficient improvement at a 80–120 mg dose level. Also, it is possible that a longer observation period of treatment at 160 mg could yield different results [48]. However, a statistical decrease in the total PANSS and CDSS scores was observed at the end of Week 1 for a dose of lurasidone of 80 mg per day. This suggests that treatment for exacerbations of schizophrenia, associated with depression, should be started at 80 mg per day; the dose should then be gradually increased based on effectiveness, safety, and tolerability. The largest reduction in the total PANSS and CDSS scores with lurasidone at 120 mg per day was associated with the best survival rate and the longest median time from treatment or follow-up initiation to discontinuation.
Our results confirm that lurasidone carries a low risk of weight gain, metabolic disorders, movement or serotonergic disorders. The most commonly reported side effects (e.g., nausea, akathisia, tremor, and drowsiness) in our study were consistent with the known drug safety profile. For example, the frequency of akathisia was 13%; nausea — 11%; tremor — 8%; and drowsiness and headache — 7%. All adverse events were mild or moderate. At the same time, lurasidone at a dose of 120 mg per day was not associated with a higher frequency or severity of adverse events compared to a dose of 80 mg per day. The lurasidone safety profile is consistent with previously published RCT data [38, 41, 49].
Study limitations
To date, there exist a variety of views on the combination of depression and schizophrenia and their clinical signs. This leads to possible clinical and psychopathological diversity amongst study results. It may be related to the individual variability in the effect of lurasidone. This study was not blinded and did not include a control group. We suspect that the improvement in depression was the result of the positive effect deriving from participation in the observational study itself or the expectation of a positive result by the physician, rather than as a direct effect of the drug. At the same time, patients continued to receive their standard psychiatric care and management without any additional research interventions. Limitations also include the relatively short duration of the follow-up period. Then, further studies on the long-term effectiveness of lurasidone in patients with schizophrenia and depressive symptoms are needed.
Implementation into practice
We report on the results of the first Russian multicenter observational study of the effectiveness of lurasidone in patients with acute episodes of schizophrenia and associated symptoms of depression. This study showed that six weeks of lurasidone therapy at doses of 40 to 160 mg per day provided a significant improvement in the CDSS (primary effectiveness endpoint) and PANSS (key secondary effectiveness endpoint) total scores and other secondary effectiveness endpoints (positive and negative symptom scores). We documented side effects of lurasidone such as nausea, akathisia, drowsiness, and minimal effect on body weight and metabolic parameters. These side effects are consistent with the safety profile reported in randomized controlled trials. The study confirmed that lurasidone is effective and well-tolerated in the treatment of acute episodes of schizophrenia and associated symptoms of depression.
CONCLUSION
A six-week prospective observational study of the real-world clinical effectiveness of lurasidone in doses ranging from 40 mg to 160 mg per day established statistically and clinically significant improvements in both psychotic and depressive symptoms in patients with acute exacerbation of schizophrenia and associated symptoms of depression. Lurasidone proved overall safe and well-tolerated, with little effect on weight, metabolic, or endocrine parameters, and even on the neurological status of the patients.
References
- Lindenmayer JP, Grochowski S, Kay SR. Schizophrenic patients with depression: psychopathological profiles and relationship with negative symptoms. Compr Psychiatry. 1991 Nov-Dec;32(6):528–533. doi: 10.1016/0010-440x(91)90032-8
- Siris SG. Depression in schizophrenia: perspective in the era of “Atypical” antipsychotic agents. Am J Psychiatry. 2000 Sep;157(9):1379–1389. doi: 10.1176/appi.ajp.157.9.1379
- Majadas S, Olivares J, Galan J, Diez T. Prevalence of depression and its relationship with other clinical characteristics in a sample of patients with stable schizophrenia. Compr Psychiatry. 2012 Feb;53(2):145–151. doi: 10.1016/j.comppsych.2011.03.009
- Miura I, Nosaka T, Yabe H, Hagi K. Antidepressive Effect of Antipsychotics in the Treatment of Schizophrenia: Meta-Regression Analysis of Randomized Placebo-Controlled Trials. Int J Neuropsychopharmacol. 2021 Mar 17;24(3):200–215. doi: 10.1093/ijnp/pyaa082
- Liu R, Fang X, Yu L, Wang D, Wu Z, Guo C, Teng X, Ren J, Zhang C. Gender Differences of Schizophrenia Patients With and Without Depressive Symptoms in Clinical Characteristics. Front Psychiatry. 2021;12:792019. doi: 10.3389/fpsyt.2021.792019
- Upthegrove R, Marwaha S, Birchwood M. Depression and Schizophrenia: Cause, Consequence, or Trans-diagnostic Issue? Schizophr Bull. 2017 Mar 1;43(2):240–244. doi: 10.1093/schbul/sbw097
- Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, Malaspina D, Owen MJ, Schultz S, Tsuang M, et al. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013 Oct;150(1):3–10. doi: 10.1016/j.schres.2013.05.028
- Reininghaus U, Bohnke JR, Hosang G, Farmer A, Burns T, McGuffin P, Bentall RP. Evaluation of the validity and utility of a transdiagnostic psychosis dimension encompassing schizophrenia and bipolar disorder. Br J Psychiatry. 2016 Aug;209(2):107–113. doi: 10.1192/bjp.bp.115.167882
- Reininghaus U, Bohnke JR, Chavez-Baldini U, Gibbons R, Ivleva E, Clementz BA, Pearlson GD, Keshavan MS, Sweeney JA, Tamminga CA. Transdiagnostic dimensions of psychosis in the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP). World Psychiatry. 2019 Feb;18(1):67–76. doi: 10.1002/wps.20607
- Tamminga CA, Ivleva EI, Keshavan MS, Pearlson GD, Clementz BA, Witte B, Morris DW, Bishop J, Thaker GK, Sweeney JA. Clinical phenotypes of psychosis in the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP). Am J Psychiatry. 2013 Nov; 170(11):1263–1274. doi: 10.1176/appi.ajp.2013.12101339
- Krynicki CR, Upthegrove R, Deakin JFW, Barnes TRE. The relationship between negative symptoms and depression in schizophrenia: a systematic review. Acta Psychiatr Scand. 2018 May;137(5):380–390. doi: 10.1111/acps.12873
- An der Heiden W, Leber A, Hafner H. Negative symptoms and their association with depressive symptoms in the long-term course of schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2016 Aug;266(5):387–396. doi: 10.1007/s00406-016-0697-2
- Felmet K, Zisook S, Kasckow JW. Elderly patients with schizophrenia and depression: diagnosis and treatment. Clin Schizophr Relat Psychoses. 2011 Jan;4(4):239–250. doi: 10.3371/CSRP.4.4.4
- Jhawer H, Sidhu M, Patel RS. Missed Diagnosis of Major Depressive Disorder with Catatonia Features. Brain Sci. 2019 Feb 2;9(2):31. doi: 10.3390/brainsci9020031
- Borisova PO. Nosological Dilemma and Clinical Polymorphism of the Catatonia Phenomenon. Psychiatry. 2020;18(2):61–70. doi: 10.30629/2618-6667-2020-18-2-61-70
- Mazo GE, Gorbachyov SE. [Depression in schizophrenia: experiences and approaches to diagnosis and treatment in psychiatric practice]. Socialnaja i klinicheskaja psihiatrija. 2009;19(4):5–14. Russian.
- Helfer B, Samara MT, Huhn M, Klupp E, Leucht C, Zhu Y, Engel RR, Leucht S. Efficacy and Safety of Antidepressants Added to Antipsychotics for Schizophrenia: A Systematic Review and Meta-Analysis. Am J Psychiatry. 2016 Sep 1;173(9):876–886. doi: 10.1176/appi.ajp.2016.15081035
- Gregory A, Mallikarjun P, Upthegrove R. Treatment of depression in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2017 Oct;211(4):198–204. doi: 10.1192/bjp.bp.116.190520
- Dorofeikova MV, Petrova NN. [Personalised approach to therapy of depression of schizophrenia]. Modern therapy of mental disorders. 2021;(3):32–44. Russian. doi: 10.21265/PSYPH.2021.99.14.004
- psychiatr.ru site of the Russian Society of Psychiatrists [Internet]. Federal clinical guidelines for the diagnosis and treatment of schizophrenia [cited 22 June 2022]. Available from: http://psychiatr.ru/download/1269.
- Whitehead C, Moss S, Cardno A, Lewis G. Antidepressants for the treatment of depression in people with schizophrenia: a systematic review. Psychol Med. 2003 May;33(4):589–599. doi: 10.1017/s0033291703007645
- Bosanac P, Castle DJ. Schizophrenia and depression. Med J Aust. 2013 Sep 16;199(S6):S36–39. doi: 10.5694/mja12.10516
- Tapp A, Kilzieh N, Wood AE, Raskind M, Tandon R. Depression in patients with schizophrenia during an acute psychotic episode. Compr Psychiatry. 2001 Jul-Aug;42(4):314–318. doi: 10.1053/comp.2001.24577
- Ishibashi T, Horisawa T, Tokuda K, Ishiyama T, Ogasa M, Tagashira R, Matsumoto K, Nishikawa H, Ueda Y, Toma S, et al. Pharmacological profile of lurasidone, a novel antipsychotic agent with potent 5-hydroxytryptamine 7 (5-HT7) and 5-HT1A receptor activity. J Pharmacol Exp Ther. 2010 Jul;334(1):171–181. doi: 10.1124/jpet.110.167346
- Citrome L. Schizophrenia relapse, patient considerations, and potential role of lurasidone. Patient Prefer Adherence. 2016;10:1529–1537. doi: 10.2147/PPA.S45401
- Murai T, Nakako T, Ikeda K, Ikejiri M, Ishiyama T, Taiji M. Lack of dopamine D4 receptor affinity contributes to the procognitive effect of lurasidone. Behav Brain Res. 2014 Mar 15;261:26–30. doi: 10.1016/j.bbr.2013.11.036
- Caccia S, Pasina L, Nobili A. Critical appraisal of lurasidone in the management of schizophrenia. Neuropsychiatr Dis Treat. 2012;8:155–168. doi: 10.2147/NDT.S18059
- Mauri MC, Paletta S, Maffini M, Colasanti A, Dragogna F, Di Pace C, Altamura AC. Clinical pharmacology of atypical antipsychotics: an update. EXCLI J. 2014;13:1163–1191.
- Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, Arndt T, Backers L, Rothe P, Cipriani A, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019 Sep 14;394(10202):939–951. doi: 10.1016/S0140-6736(19)31135-3
- Meyer JM, Mao Y, Pikalov A, Cucchiaro J, Loebel A. Weight change during long-term treatment with lurasidone: pooled analysis of studies in patients with schizophrenia. Int Clin Psychopharmacol. 2015 Nov;30(6):342–350. doi: 10.1097/YIC.0000000000000091
- Meyer JM, Ng-Mak DS, Chuang CC, Rajagopalan K, Loebel A. Weight changes before and after lurasidone treatment: a real-world analysis using electronic health records. Ann Gen Psychiatry. 2017;16:36. doi: 10.1186/s12991-017-0159-x
- Riva MA, Albert U, de Filippis S, Vita A, De Berardis D. Identification of clinical phenotypes in schizophrenia: the role of lurasidone. Ther Adv Psychopharmacol. 2021;11:20451253211012250. doi: 10.1177/20451253211012250
- Nakamura M, Ogasa M, Guarino J, Phillips D, Severs J, Cucchiaro J, Loebel A. Lurasidone in the treatment of acute schizophrenia: a double-blind, placebo-controlled trial. J Clin Psychiatry. 2009 Jun;70(6):829–836. doi: 10.4088/JCP.08m04905
- Meltzer HY, Cucchiaro J, Silva R, Ogasa M, Phillips D, Xu J, Kalali AH, Schweizer E, Pikalov A, Loebel A. Lurasidone in the treatment of schizophrenia: a randomized, double-blind, placebo- and olanzapine-controlled study. Am J Psychiatry. 2011 Sep;168(9):957–967. doi: 10.1176/appi.ajp.2011.10060907
- Nasrallah HA, Cucchiaro JB, Mao Y, Pikalov AA, Loebel AD. Lurasidone for the treatment of depressive symptoms in schizophrenia: analysis of 4 pooled, 6-week, placebo-controlled studies. CNS Spectr. 2015 Apr;20(2):140–147. doi: 10.1017/S1092852914000285
- Loebel A, Cucchiaro J, Xu J, Sarma K, Pikalov A, Kane JM. Effectiveness of lurasidone vs. quetiapine XR for relapse prevention in schizophrenia: a 12-month, double-blind, noninferiority study. Schizophr Res. 2013 Jun;147(1):95–102. doi: 10.1016/j.schres.2013.03.013
- Marder SR, Davis JM, Chouinard G. The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis: combined results of the North American trials. J Clin Psychiatry. 1997 Dec;58(12):538–546. doi: 10.4088/jcp.v58n1205
- Hopkins SC, Ogirala A, Loebel A, Koblan KS. Transformed PANSS Factors Intended to Reduce Pseudospecificity Among Symptom Domains and Enhance Understanding of Symptom Change in Antipsychotic-Treated Patients With Schizophrenia. Schizophr Bull. 2018 Apr 6;44(3):593–602. doi: 10.1093/schbul/sbx101
- Harvey PD, Siu CO, Loebel AD. Insight and Treatment Outcomes in Schizophrenia: Post-hoc Analysis of a Long-term, Double-blind Study Comparing Lurasidone and Quetiapine XR. Innov Clin Neurosci. 2017 Dec 1;14(11–12):23–29.
- Oleichik IV, Baranov PA, Shishkovskaia TI, Sizov SV. Efficacy and Safety of the Third-Generation Atypical Antipsychotic Lurazidone in the Treatment of Depression in Schizophrenia. Current Therapy of Mental Disorders. 2021;(2):28–35. Russian. doi: 10.21265/PSYPH.2021.57.2.004
- Rajagopalan K, Wade S, Meyer N, Loebel A. Real-world adherence assessment of lurasidone and other oral atypical antipsychotics among patients with schizophrenia: an administrative claims analysis. Curr Med Res Opin. 2017 May;33(5):813–820. doi: 10.1080/03007995.2017.1284656
- Loebel A, Cucchiaro J, Silva R, Kroger H, Hsu J, Sarma K, Sachs G. Lurasidone monotherapy in the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry. 2014 Feb;171(2):160–168. doi: 10.1176/appi.ajp.2013.13070984
- Loebel A, Cucchiaro J, Silva R, Kroger H, Sarma K, Xu J, Calabrese JR. Lurasidone as adjunctive therapy with lithium or valproate for the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry. 2014 Feb;171(2):169–177. doi: 10.1176/appi.ajp.2013.13070985
- Maslennikov NV, Cukarzi EE, Mosolov SN. Algorithm for biological therapy of depression in schizophrenia. Current therapy of mental disorders. 2019;(2):31–40. Russian. doi: 10.21265/PSYPH.2019.34.92.005
- Amri I, Millier A, Toumi M. Minimum Clinically Important Difference in the Calgary Depression Scale for Schizophrenia. Value Health. 2014 Nov;17(7):A766. doi: 10.1016/j.jval.2014.08.288
- Addington J, Shah H, Liu L, Addington D. Reliability and validity of the Calgary Depression Scale for Schizophrenia (CDSS) in youth at clinical high risk for psychosis. Schizophr Res. 2014 Mar;153(1–3):64–67. doi: 10.1016/j.schres.2013.12.014
- Ivanova E, Khan A, Liharska L, Reznik A, Kuzmin S, Kushnir O, Agarkov A, Bokhan N, Pogorelova T, Khomenko O, et al. Validation of the Russian Version of the Positive and Negative Syndrome Scale (PANSS-Ru) and Normative Data. Innov Clin Neurosci. 2018 Oct 1;15(9–10):32–48.
- Loebel A, Silva R, Goldman R, Watabe K, Cucchiaro J, Citrome L, Kane JM. Lurasidone Dose Escalation in Early Nonresponding Patients With Schizophrenia: A Randomized, Placebo-Controlled Study. J Clin Psychiatry. 2016 Dec;77(12):1672–1680. doi: 10.4088/JCP.16m10698
- Goldman R, Loebel A, Cucchiaro J, Deng L, Findling RL. Efficacy and Safety of Lurasidone in Adolescents with Schizophrenia: A 6-Week, Randomized Placebo-Controlled Study. J Child Adolesc Psychopharmacol. 2017 Aug;27(6):516–525. doi: 10.1089/cap.2016.0189
Information About the Authors
Metrics
Web Views
Whole time: 702
Previous month: 31
Current month: 33
PDF Downloads
Whole time: 101
Previous month: 7
Current month: 2
Total
Whole time: 803
Previous month: 38
Current month: 35